|
|
|
|
|
Video-Assisted Thoracoscopic Resection of a Large Bronchogenic Cyst in a 12-Year-Old Child
|
|
|
|
Roman Dutta1, Pramoj Jindal1, Yogesh Jhamb2, Gautam Jain2 Departments of 1Thoracic & Robotic Thoracic Surgery and 2General and Minimal Access Surgery, Max Super Specialty Hospital, Vaishali, Delhi-NCR, India. |
|
|
|
|
|
Corresponding Author:
|
|
Dr. Roman Dutta Email: romandutta@gmail.com |
|
|
|
|
|
|
|
|
Received:
14-JUL-2022 |
Accepted:
08-MAY-2023 |
Published Online:
25-SEP-2023 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
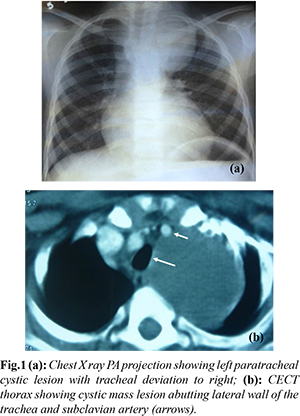
Background: We present a rare case of a 12-year-old male child with seizures, chest pain, fever, cough, and breathing difficulty, revealing a large cystic lesion in the left paratracheal chest region. Coexisting tubercular lesions in the brain complicated the diagnosis. The patient had been under anti-tubercular treatment prior to admission. Case Report: A Video-assisted Thoracoscopic Surgery (VATS) was performed, excising the 8×7 cm cyst causing partial collapse of the left upper lobe lung. The cyst, intricately connected to the tracheal wall and vascularized by the left subclavian artery, was meticulously dissected, aspirated, and removed. Post-surgery, the patient recovered well, with the chest tube removed on the second day. Follow-up imaging confirmed lung expansion, and the patient was discharged on the third post-operative day. Conclusion: VATS proved to be an effective and minimally invasive technique for the excision of a large bronchogenic cyst, ensuring a rapid recovery and excellent long-term outcomes. This case highlights the significance of multidisciplinary approaches and precise surgical techniques in managing such intricate cases in young patients. |
|
|
|
|
|
Keywords :
|
Bronchogenic Cyst, Chest Tube, Chest Pain, Cough, Thoracoscopy.
|
|
|
|
|
|
|
|
|
|
|
|
Introduction
Bronchogenic cysts may typically occur in any part of the mediastinum, but majority arise in close proximity to the trachea, main bronchi and carina. They are identified in all age groups. Bronchogenic cysts are mostly asymptomatic and present as an incidental finding on routine chest X-ray or CT scans. Bleeding, infection or epithelial secretions may cause cyst enlargement and symptomatic compression of the aero digestive tract, resulting in chest pain, cough, dyspnea, fever and pneumonia. Most surgeons would recommend early excision of the cyst even in an asymptomatic patient. Minimally invasive techniques, such as Video-assisted Thoracoscopic Surgery (VATS), have revolutionized the surgical management of mediastinal cysts through reduced post-operative pain, shorter hospital stays, and faster recovery, making it particularly important in pediatric cases where minimizing trauma is paramount. We hereby emphasize the efficacy and safety of VATS as an optimal surgical modality of pediatric thoracic surgery.
Case Report
We hereby report a 12-year-old male child who was admitted to the hospital due to a series of symptoms, including seizures, chest pain, intermittent fever, productive cough, and difficulty in breathing. Upon further evaluation for the seizures, a large cystic lesion located in the left paratracheal region of the chest was discovered. The presence of this lesion was also associated with a tubercular lesion in the brain, as observed in an MRI scan. The patient had been undergoing treatment with oral anti-tubercular drugs for six months prior to admission, based on the advice of a physician. A preliminary chest X-ray (PA view) revealed the presence of a large cystic lesion [Fig.1a], which was subsequently confirmed and further characterized using contrast-enhanced computed tomography of the chest [Fig.1b]. The cyst, measuring 8×7 cm, was causing partial collapse of the left upper lobe lung and was symptomatic, necessitating intervention.
The patient underwent Video-assisted Thoracoscopic Surgery (VATS) for exploration and complete excision of the cyst. Under general anaesthesia and with selective one-lung ventilation facilitated by a double lumen endotracheal tube, the procedure was performed. Three ports were created for endoscope insertion and operating instruments. The cyst, firmly adherent to the lateral wall of the trachea, was carefully dissected out [Fig.2a]. It was found to be receiving blood supply from the left subclavian artery [Fig.2b], which was clipped and divided. The cyst contained thick, milky-coloured material, which was aspirated before the cyst was excised [Fig.2c]. The excised cyst was placed in an endo bag and removed through one of the ports [Fig.2d]. Following the surgery, the patient's chest tube was removed on the second day post-operation, and a chest X-ray revealed expanded lung capacity. The patient recovered well and was discharged from the hospital on the third day after the surgery. Subsequent follow-up examinations over the past 72 months have shown the patient to be in good health.
Discussion
Bronchogenic cysts are rare developmental anomaly of embryonic foregut. Bronchogenic cyst arises from abnormal branching or budding of the trachea-bronchial tree. In the presence of persistent bronchial communication, they are either intra-parenchymal or in close proximity to lung. The subset of the cyst, which does not communicate with the airway, gradually distends due to accumulation of its secretions. The cyst becomes symptomatic due to pressure symptoms in surrounding structures or when they are secondarily infected. Infections in bronchogenic cyst present like an intra-thoracic abscess [ 1]. There is no universal consensus about the management of the bronchogenic cyst. However, since the classic description of bronchogenic cyst by Mayer et al, most of the surgeons recommend surgical resection of the bronchogenic cyst due to its potential for complications as a result of infection in the cyst or gradual increase in size. Surgical excision offers complete and definitive treatment, eliminate potential for complications and provide histological diagnosis [1-3]. The presented case illuminates the intricate nature of pediatric bronchogenic cysts, compounded by their rare co-existence with tubercular lesions in the brain. Traditional thoracotomy provides excellent exposure of the cyst and its relations with surrounding structure. Thoracic surgeons have used VATS to perform cyst excision with outstanding success [4,5]. The successful application of VATS in our case underscores its effectiveness in managing such complex conditions. VATS, with its minimally invasive approach, allowed meticulous dissection of the cyst, resolving the respiratory distress caused by the cyst. We found aspiration of the thick milky content of the cyst at the beginning of the VATS procedure immensely helpful as it provides ample space for the operating instruments in narrow space like apex of the thoracic cavity. Bronchogenic cyst can be adherent to the wall of the tracheobronchial tree due to dense fibrotic reaction surrounding the cyst. Therefore, operating surgeon need to be careful to prevent damage to the tracheobronchial tree. The identification and management of the cyst's vascular supply, a crucial step in preventing intraoperative complications, were achieved successfully. In our patient the wall of the cyst was adherent to the left subclavian artery (SA) from which it was carefully dissected out to identify the feeder vessel for ligation.
Conclusion
Our experience reaffirms that VATS is a safe and effective approach in the treatment of large bronchogenic cysts in pediatric patients, even in the presence of complicating factors such as concomitant intracranial pathology.
Contributors: RD, PJ: manuscript writing, surgical management; YJ, GJ: manuscript editing, patient management. RD will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study. Funding: None; Competing interests: None stated.
References - Maier HC. Bronchiogenic cysts of the mediastinum. Ann Surg. 1948;127(3):476-502.
- Cioffi U, Bonavina L, De Simone M, Santambrogio L, Pavoni G, Testori A, et al. Presentation and surgical management of bronchogenic and esophageal duplication cysts in adults. Chest. 1998;113:1492.
- Kanemitsu Y, Nakayama H, Asamura H, Kondo H, Tsuchiya R, Naruke T. Clinical features and management of bronchogenic cysts: report of 17 cases. Surg Today. 1999;29(11):1201-1205.
- Jung HS, Kim DK, Lee GD, Sim HJ, Choi SH, Kim HR, et al. Video-assisted thoracic surgery for bronchogenic cysts: Is this the surgical approach of choice? Interact Cardiovasc Thorac Surg. 2014;19(5):824-829.
- Mouroux J, Bourgeon A, Benchimal D, Bernard JL, Chazal M, Padovani B, et al. Bronchogenic cysts of the esophagus. Classical surgery or video-surgery? Chirurgie. 1991;117:564-568.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Dutta R, Jindal P, Jhamb Y, Jain GVideo-Assisted Thoracoscopic Resection of a Large Bronchogenic Cyst in a 12-Year-Old Child.JCR 2023;13:98-100 |
|
Dutta R, Jindal P, Jhamb Y, Jain GVideo-Assisted Thoracoscopic Resection of a Large Bronchogenic Cyst in a 12-Year-Old Child.JCR [serial online] 2023[cited 2024 Dec 21];13:98-100. Available from: http://www.casereports.in/articles/13/3/Video-Assisted-Thoracoscopic-Resection-of-a-Large-Bronchogenic-Cyst-in-a-12-Year-Old-Child.html |

|
|
|
|
|