Introduction
Pregnancy developing in a cesarean scar site is the rarest form of ectopic pregnancy, with a prevalence of approximately one case per 2000 ectopic pregnancies. This condition poses significant diagnostic and management challenges, and if not diagnosed and treated early, it can lead to severe maternal morbidity and mortality [1]. The incidence of cesarean scar ectopic pregnancies is rising in parallel with the increase in primary and repeat cesarean sections, which globally account for about 18.6% of all births [2].
There are two types of cesarean scar ectopic pregnancies: Type 1, which grows into the uterine cavity (endogenous CSP), and Type 2, which grows towards the bladder or abdominal cavity (exogenous CSP). Exogenous CSP has a worse prognosis due to the risk of spontaneous uterine rupture, hemorrhage, and maternal death. Accurate and timely diagnosis is crucial.
Case Report
This case report describes a 35-year-old female, Gravida 3, Para 1, with one living child and one previous abortion. She presented with one and a half months of amenorrhea but no vaginal bleeding or abdominal pain. A home urine pregnancy test was positive, and during a routine antenatal visit to a private hospital, an ultrasound scan incidentally detected a cesarean scar pregnancy, showing a single live intrauterine gestation corresponding to a 6-week gestational sac in the lower uterine segment. She was referred to our medical center for a second opinion. A repeat ultrasound confirmed the diagnosis [Fig.1,2].
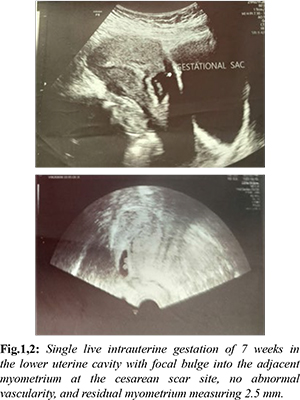
Upon admission to the Department of Obstetrics and Gynaecology, routine investigations, including liver and renal function tests and beta HCG levels, were conducted. High-risk consent regarding potential uterine rupture and maternal mortality was obtained. Initial beta HCG was 50,539 mIU/mL, and other test results were within normal limits. An MRI of the pelvis [Fig.3] showed a gestational sac of 2.8 cm in diameter in the lower uterine region, near the serosal surface, suggesting implantation in the anterior uterine wall at the scar site.

Repeat investigations showed beta HCG at 63,689 mIU/mL. Despite the administration of methotrexate and folinic acid, the beta HCG levels and ultrasound findings indicated that the ectopic pregnancy persisted with fetal cardiac activity. Given the failure of medical treatment, the patient underwent an elective laparotomy. The procedure involved the removal of the gestational sac and a bilateral tubectomy. Dense adhesions between the anterior abdominal wall and uterus were lysed, and a vertical incision on the previous cesarean scar site allowed the gestational sac and fetus to be removed. The gestational sac and membranes were sent for histopathological examination, which confirmed the presence of products of conception. The patient's postoperative period was uneventful.
Discussion
Cesarean scar ectopic pregnancy (CSP) is the rarest form of ectopic pregnancy. We report the case of a 35-year-old female who presented incidentally with a cesarean scar ectopic pregnancy. Medical management was attempted but failed, necessitating a laparotomy with removal of the gestational sac and bilateral tubectomy.
One case series indicates that most cesarean scar ectopic pregnancies occur after only one cesarean section, suggesting that the number of cesarean sections may not be an independent risk factor [2]. Similarly, our patient had a history of just one previous cesarean section. For women with a cesarean section history, the frequency of CSP is approximately 0.15%, accounting for 6.1% of all ectopic pregnancies in this group [3-6].
Various theories explain the etiology and mechanism of cesarean scar ectopic pregnancy, with the most accepted being that the blastocyst invades the myometrium through a microscopic dehiscent tract, often resulting from previous uterine surgeries like cesarean sections or manual placenta removal [3]. Upon implantation in the uterine scar, CSP can extend either into the cervico-isthmic space and the uterine cavity or deeper into the myometrium toward the serosal surface of the uterus. Both scenarios can result in substantial hemorrhage, with the latter precluding a viable pregnancy [5]. For stable patients, uterine artery embolization and expectant management are options but require close follow-up to avoid potential complications such as uterine rupture. Surgical treatment, successful in 96% of cases, is the most definitive option, as it removes the gestation, repairs the uterine defect, and preserves future fertility [2]. In a study by Parihar et al., medical management was initially attempted, but persistence of the gestational sac required subsequent suction evacuation. Combining medical management with curettage can be highly successful and reduce intraoperative blood loss [4]. However, the risk of hemorrhage during curettage is influenced by gestational age and sac size.
This case emphasizes the importance of considering cesarean scar ectopic pregnancies in the differential diagnosis for pregnant women with a history of cesarean section, whether detected incidentally or presenting with vaginal bleeding. Women should be counselled about the increased risk of developing CSP due to prior uterine surgery.
Conclusion
A viable cesarean scar pregnancy can be surgically managed when medical management fails. The choice of treatment should be based on gestational age, human chorionic gonadotropin levels, cardiac activity, the patient's desire for future fertility, and the available medical facilities. Early diagnosis can often lead to successful medical management, but some cases may ultimately require surgical intervention.
Contributors: GBS: manuscript writing, patient management; PSS: manuscript editing, patient management; RP: critical inputs into the manuscript. GBS will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Jameel K, Abdul Mannan GE, Niaz R, Hayat DE. Cesarean scar ectopic pregnancy: A diagnostic and management challenge. Cureus. 2021;13(4):e14463.
- Majangara R, Madziyire MG, Verenga C, Manase M. Cesarean section scar ectopic pregnancy - a management conundrum: a case report. J Med Case Rep. 2019;13(1):137
- Deepika, Gupta T, Wahi S. A rare case report of caesarean scar ectopic pregnancy. J Clin Diagn Res. 2017;11(8):QD10-QD11.
- Parihar P, Gupta M, Kapoor P, Preeti, Minhas S. Caesarean scar ectopic pregnancy: A case successfully managed using systemic methotrexate and suction and evacuation. J Clin Diagn Res. 2021;15(11):3-5.
- Brancazio S, Saramago I, Goodnight W, McGinty K. Cesarean scar ectopic pregnancy: Case report. Radiol Case Rep. 2019;14(3):354-359.
- Fowler ML, Little S, Muto M, Mahalingaiah S. Mid-trimester cesarean scar pregnancy: a case report. Fertil Res Pract. 2021;7(1):10.
- Gupta N, Barbaraa H, Kennethb E, Josefa B. Cesarean scar ectopic pregnancy. J Clin Gynecol Obstet. 2013;2(1):42-44.
- Heidar Z, Zade h Modarres S, Abediasl Z, Khaghani A, Salehi E, Esfidani T. Cesarean scar pregnancy treatment: a case series. J Med Case Reports. 2021;15:506.
- Kim DJ, Welch M, Kendall JL. A case of cesarean scar ectopic: a rare but important form of ectopic pregnancy. Crit Ultrasound. 2011;3:55-57.
- Smith DJ, Chenkin J. Cesarean scar ectopic pregnancy diagnosed by point-of-care ultrasound: A case report. CJEM. 2020;22(5):723-725.