Introduction
Impalement injuries are defined as injuries that are caused by a foreign object penetrating the body of a person [
1]. These objects may penetrate up to varying depths in the body or may pass through and through depending on factors like velocity of impact and resistance offered by the body to the penetrating object [
2]. Impalement injuries are uncommonly encountered injuries in our day-to-day emergency department. Thus, not all residents and faculty are exposed to such cases which require reporting varying types of impalement injuries, what led to these injuries, their management, outcome and educating the general public an essential part of the process. Multiple case reports on impalement injuries to thorax and abdomen have been demonstrated however less than ten case reports have been reported for upper limb impalement injuries [
3-
6]. We hereby present successful management of left forearm impalement injury.
Case Report
Our patient was a 38-year-old male, who presented to us with impalement injury to left forearm with a spearhead iron fence. The patient who was under alcohol influence at the time of injury was climbing stairs having unsupported railings during which his leg slipped and he fell on an iron fence directly near the staircase leading to impalement of one of the rods into his left forearm. Our patient belonged to a remote village in Central India. The incident occurred at 11:00 pm. As the patient was stuck to the iron gate, he held onto the gate with his other hand and called for help immediately. His neighbors successfully managed to separate the iron fence rod stuck in his left forearm from the gate, however it took two hours’ effort on their part to do the job. The patient only presented to us at around 5:00 am in our emergency department which is the closest tertiary care center to their village.
Our examination findings were as follows. Patient was conscious and oriented at the time of presentation. He had a pulse of 110/min and BP was 130/80 mm of Hg. According to the history given, the patient did not lose excessive blood at the time of injury and transport. There were no other associated injuries. An iron rod was seen entering through the ulnar aspect of left forearm with muscle protruding through the entry point and no exit of rod through the radial aspect [Fig.1]. There was restriction of flexion at proximal interphalangeal joints of ring and little finger. Both radial and ulnar arteries were palpable, and sensations were intact. His X-ray was suggestive of no bony injury. Tetanus prophylaxis was given.

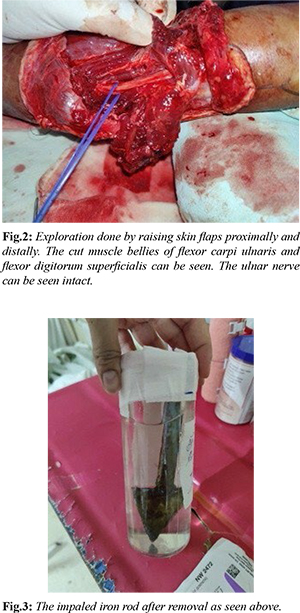
The patient was immediately taken under general anesthesia. Exploration of the wound was done by raising the skin flaps proximally and distally. The iron rod was removed under vision. Ulnar artery and nerve, median nerve was found to be intact [Fig.2]. The cut and contaminated ends of muscle bellies were debrided. Thorough wash with betadine solution and normal saline was given. The cut muscle bellies of flexor digitorum superficialis and flexor carpi ulnaris were repaired, followed by placement of drain and skin closure. The patient was given an above elbow splint with elbow flexion and hand in dorsal blocking position. The iron rod after removal is shown in Fig.3.
The patient was admitted for a duration of 5 days during which he received intravenous antibiotics. Drain was removed on post-operative day 2. Patient developed partial flap necrosis however there was no progression seen on day 4 which later healed spontaneously. After discharge, the patient was advised weekly follow up for physiotherapy. Daytime splint was discontinued after 6 weeks and nighttime after 8 weeks. Patient regained complete range of motion in 3 months duration.
Discussion
Impalement injuries have been classified into two types: Type 1, where a mobile human body hits a stationary object, and Type 2, where a moving object hits a stationary human body [
7]. Impalement injuries can either be simple or complex. Simple injury is due to type 2 injury. A type 1 injury leads to a complex injury wherein the human body is fixed to a larger object which needs to be cut short at the entry point to allow the patient to be transported to the hospital [
7].
Our patient had a type 1 complex injury. These impalement injuries are more commonly seen in the trunk which has a larger area of contact as compared to extremities which have smaller area and is more mobile. Thus, the impalement injuries in extremities are more by a thinner and sharper object [5]. Any attempt to remove the impaled object from the patient’s body at the time of injury may cause significant bleeding and further tissue trauma. Hence, it is prudent on the part of rescuers to carefully cut the large, impaled object to a shorter length keeping the impaled object stable in the patient’s body to allow for transportation [8]. These injuries may pose a great challenge in transporting patients with the impaled object from distant villages to the major tertiary care centers in India. The most life-threatening condition would be excessive hemorrhage at the time of injury and hemodynamic instability by the time patient along with the impaled object is separated to allow transportation. Another significant risk is dislodgement of the impaled object while separating the patient with impaled object or during transportation leading to hemorrhage in case of vascular injury. All this added to the increased duration of transport makes it a challenge for both the rescuers and the managing doctors. In a country like India in remote villages, the primary rescuers are the patient’s family members and neighbors. Thus, educating the masses regarding primary care in case of such injuries is essential to reduce morbidity and prevent mortality.
The following are the guidelines to be followed in case of impalement injury to extremities. Once a patient presents to an emergency department, the first step would be to manage the hemodynamic instability and rule out other injuries [9]. Both anti-tetanus serum and booster dose of tetanus should be administered along with broad spectrum antibiotics as per guidelines [10]. After the patient is stabilized, radiological and necessary blood investigations should be carried out. Patients should be taken under limb block or general anesthesia. The impaled object should be removed only under vision; hence the incisions should be extended for adequate exposure. After the removal of the impaled object, generous debridement and thorough wash is essential to prevent infection at a later stage [1]. Adequate hemostasis should be achieved. Repair of the cut structures should be followed by splintage and limb elevation in the post-operative period. Antibiotics should be given for 5-7 days in the post-operative period. Be vigilant about any infection or discharge from the wound. Early mobilization and regular follow-up are also important.
Conclusion
Thus, by educating the masses in managing the pre-hospital course and rapid early surgical intervention by the hospital personnel, we can successfully manage impalement injuries to extremities with minimal morbidity, mortality, and good functional outcomes.
Contributors: KNK: conceptualization and preparation of manuscript; SBP: manuscript review; NG: references and literature search; VSB: photographs and manuscript preparation; SSD: critical inputs into the manuscript. KNK will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Horowitz MD, Dove DB, Eismont FJ, Green BA. Impalement injuries. J Trauma. 1985;25(9):914-916.
- Goel T. Case report of isolated impaling lung injury with successful outcome. Int Surg J. 2017;4(10):3548-3551.
- Singh SB, Jain A, Singh AK. Unusual injuries of the hand: Impalement injuries. Arch Trauma Res. 2021;10:173-175.
- Ohn MH, Ohn KM. A case of impalement injury of finger. BMJ Case Rep. 2020;13(12):e239234.
- Elamurugan T, Sreenath G, Jagdish S. An unusual impalement injury involving both extremities. African J Trauma. 2014;3:91-93.
- Kelly IP, Attwood SE, Quilan W, Fox MJ. The management of impalement injury. Injury. 1995;26(3):191-193.
- Govindaraju RC, Munavalli J. Difficulties in the management of impalement injuries sustained in Rural India. Journal of Emergencies, Trauma, and Shock. 2020;13(3):227-230.
- Greenberg MI. The diagnosis: Impalement injury. Emergency Medicine News. 2001;23(9):20.
- Hyde MR, Schmidt CA, Jacobson JG, Vyhmeister EE, Laughlin LL. Impalement injuries to the thorax as a result of motor vehicle accidents. Ann Thorac Surg. 1987;43(2):189-190.
- Banshelkikar SN, Sheth BA, Dhake RP, Goregaonkar AB. Impalement injury to thigh: A case report with review of literature. J Orthop Case Rep. 2018;8(1):71-74.