|
|
|
|
|
Rare Presentation of Intramuscular Hemangioma: A Case Series
|
|
|
|
Priya N, Jayanthi C, Vimal M, Srivani S Department of Pathology, Sri Manakula Vinayagar Medical College and Hospital, Pondicherry. India. |
|
|
|
|
|
Corresponding Author:
|
|
Dr Priya N Email: priyanatarajan4295@gmail.com |
|
|
|
|
|
|
|
|
Received:
14-JUN-2024 |
Accepted:
08-OCT-2024 |
Published Online:
25-DEC-2024 |
|
|
|
|
|
|
|
Abstract
|
|
|
|
Background: Intramuscular hemangiomas (IMH) are rare benign vascular tumors that present as a slow-growing, painless mass in large muscles of the trunk and extremities. IMH is frequently misdiagnosed pre-operatively, with definitive diagnosis relying on histopathology. Complete surgical excision is the preferred treatment to prevent recurrence. Case Series: We present two cases of IMH in unusual locations. The first case involved a 29-year-old female with a three-year history of a left scapular mass, which recently showed rapid growth and pain. Imaging suggested a vascular soft tissue neoplasm, and histopathology confirmed IMH with vascular proliferation and focal adipocytic clusters. The second case was a 2-year-old male with a congenital left scapular mass that enlarged over four months. Imaging indicated a benign vascular tumor, and histopathology confirmed IMH with proliferating vascular channels infiltrating muscle, along with features such as extramedullary hematopoiesis and calcifications. Both cases were treated with wide excision and reconstructive surgery, with no recurrence reported to date. Conclusion: These cases highlight the importance of considering IMH in the differential diagnosis of unusual soft tissue masses. Imaging, particularly MRI, aids in preoperative assessment, but histopathology remains the gold standard for diagnosis. Surgical excision with wide margins is critical to prevent recurrence. |
|
|
|
|
|
Keywords :
|
Excision Biopsy, Hemangioma, MRI, Neoplasm, Vascular Tumor.
|
|
|
|
|
|
|
|
|
|
|
|
Introduction
Intramuscular hemangioma (IMH) is a rare non-metastasizing benign neoplasm accounting for 0.8% of all hemangiomas [ 1]. A distinctive type of vascular tumor occurs within the skeletal muscle, mostly located in the lower extremity (muscles of the thigh) and rarely in head and neck regions. IMH is usually found as an incidental benign palpable mass, but accurate diagnosis before surgery is difficult due to non-specific symptoms, deep anatomical positions, and a low frequency of occurrence and it is very difficult to reach the diagnosis by clinical examination and radiological finding. Hence biopsy obtained by surgical excision gives the definitive diagnosis and idea about definitive treatment. Here we are presenting interesting rare cases of intramuscular hemangioma.
Case Series
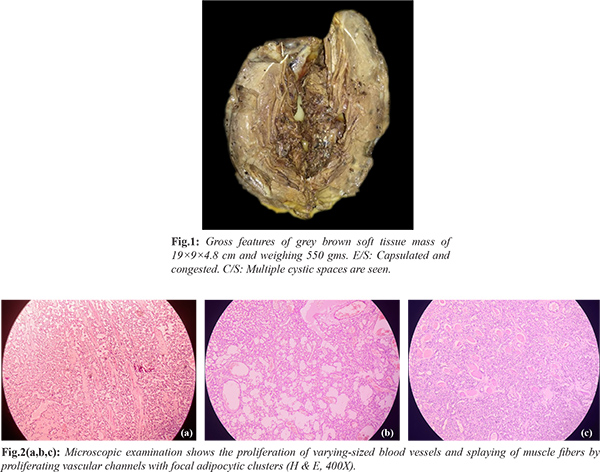
A 29-year-old female presented with a swelling on the left side of her scapula, which had been present for three years but recently showed a sudden onset of pain and a rapid increase in size over the past four months. On clinical examination, a 15×10 cm non-mobile, tender mass was identified in the left paraspinal region, leading to a provisional diagnosis of soft tissue sarcoma of the back. Imaging studies, including a CT thoracic angiogram, suggested a highly vascular soft tissue neoplasm or sarcoma, while an MRI confirmed features of a vascular soft tissue intermuscular sarcoma. Cytological findings were inconclusive. The patient underwent surgical excision of the mass using a wide excision technique with latissimus dorsi flap reconstruction, and the specimen was sent for histopathological examination. Gross evaluation of the excised mass revealed a grey-brown encapsulated soft tissue mass measuring 19×9×4.8 cm and weighing 550 grams, with multiple cystic spaces on the cut surface [Fig.1]. Microscopic examination showed the proliferation of varying-sized blood vessels and splaying of muscle fibers by vascular channels, along with focal adipocytic clusters [Fig.2]. These findings confirmed the vascular nature of the tumor.
Case 2
A 2-year-old male presented with a swelling in the upper back, noted since birth, with a sudden increase in size over the past four months. Clinical examination revealed a soft, non-mobile, non-tender mass measuring 10×8 cm in the left scapular region. The initial clinical impression was of a benign vascular tumor. Contrast-enhanced MRI confirmed the presence of a benign vascular tumor in the left scapular region, with differential diagnoses of hemangioendothelioma and hemangiopericytoma. Cytological findings revealed a vascular lesion. The patient underwent wide excision of the mass with trapezius muscle reconstruction, and the specimen was sent for histopathological evaluation. Gross examination showed a grey-brown mass with lobular architecture [Fig.3]. Microscopic analysis revealed sheets and lobules of varying-sized blood vessels within a cellular stroma, characterized by proliferating spindle cells with mild atypia. Papillary patterns, vascular channels infiltrating muscle tissue, and additional features such as extramedullary hematopoiesis, hyalinized collagenous stroma, focal calcifications, and multinucleated giant cells were observed [Fig.4,5]. These cases highlight the clinical and histopathological complexity of vascular tumors in the back, emphasizing the need for detailed evaluation to establish an accurate diagnosis and guide appropriate management.
Discussion
Intramuscular hemangiomas (IMH) are rare, comprising 0.8% of all hemangiomas and 7% of benign soft tissue tumors [ 1, 2]. First described by Liston in 1843, IMHs primarily affect young adults, often presenting before the age of 30. They typically involve the large muscles of the trunk and extremities, with rare cases in the head and neck region [ 2]. The etiology is unclear, with trauma, congenital abnormalities, and hormonal factors being potential contributors [ 3, 4]. IMH often presents as a painless, slowly growing, mobile mass without vascular signs such as skin discoloration or pulsation. However, rapid growth or pain, as seen in our cases, may indicate vascularity or infiltration. These features, combined with IMH’s rarity, lead to frequent misdiagnosis before surgery and histopathological confirmation, with less than 8% of cases accurately diagnosed preoperatively [ 5]. Our cases emphasize the diagnostic challenges of IMH. The 29-year-old female exhibited rapid tumor growth with pain, initially suggesting soft tissue sarcoma, while the 2-year-old male's painless congenital swelling was misdiagnosed as a benign vascular tumor. Preoperative imaging, particularly MRI, was pivotal in narrowing the differential diagnosis, while histopathological examination confirmed the diagnosis of IMH in both cases. IMHs are classified as capillary, cavernous, or mixed types [6]. The capillary type, the most common, is characterized by small vessels and minimal symptoms. The cavernous type involves larger vessels, often presenting with pain and a higher recurrence rate (9%) post-surgery. The mixed type, with features of both, has the highest recurrence rate and is often associated with chronic pain and swelling [6,7]. Angiomatosis usually occurs congenitally, involving large body areas and multiple tissue planes. In contrast, IMH etiology remains unknown and it occurs in the intramuscular plane with similar microscopic features in both conditions. The distinction between these conditions requires clinical input. Infantile hemangioma differs from IMH in that the former is usually seen in the skin/ soft tissues of the face, head, and neck of infants, showing lobular arrangement and proliferation of capillaries separated by thin fibrous septa with GLUT1 IHC positivity. In contrast, IMH has its common occurrence in the lower extremities. Angiolipoma occurs in the subcutaneous plane and grossly appears as a small, painful, circumscribed lesion and is often multiple. Microscopically it is composed of capillary-sized vascular channels in contrast to IMH, where cavernous type of vascular channels are seen [8]. Management depends on the tumor's size, growth, anatomical location, and patient factors. Complete surgical excision is the preferred treatment to prevent recurrence. Infiltrative tumors, as seen in our cases, often necessitate removal of adjacent normal tissue. Partial excision significantly increases recurrence rates, reported to range from 18-60% [9,10]. Adjunct treatments such as embolization can be useful in managing unresectable lesions or reducing intraoperative blood loss [11,12]. IMH does not metastasize or undergo malignant transformation.
Conclusion
Intramuscular hemangiomas are rare and often misdiagnosed due to their non-specific symptoms and low incidence. Rapid growth, pain, and imaging findings should prompt suspicion. Complete surgical excision is the treatment of choice, with careful planning to minimize recurrence. Our cases highlight the need for clinical awareness and a multidisciplinary approach to optimize outcomes.
Contributors: PN: manuscript writing, patient management; JC: manuscript editing, patient management; VM, SS: critical inputs into the manuscript. AL will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study. Funding: None; Competing interests: None stated.
References - Wild AT, Raab P, Krauspe R. Hemangioma of skeletal muscle. Archives of Orthopaedic and Trauma Surgery. 2000;120(3-4):139-143.
- Patten DK, Wani Z, Kamineni S. Intramuscular cavernous haemangioma of the triceps. Int J Surg Case Rep. 2011;2:86-89.
- Sett TK, Sett T, De S, De A, Bhar A, Basu D. Intramuscular hemangioma of triceps muscle. Indian J Basic Appl Med Res. 2014;3:467-471.
- Clemis J, Briggs D, Changus, G. Intramuscular hemangioma in the head and neck. Can J Otolaryngol. 1975;4:339-346.
- Edgerton MT. The treatment of hemangiomas: with special reference to the role of steroid therapy. Ann Surg. 1976;183:517-532.
- Wolf GT, Daniel F, Krause CJ, Kaufman RS. Intramuscular hemangioma of the head and neck. Laryngoscope. 1985;95:210-213.
- Shah SA, Hassan F. Intramuscular hemangioma of the triceps muscle. J Surg Pak (Int). 2012;17:40-42.
- Hofvander J, Arbajian E, Stenkula KG, Lindkvist-Petersson K, Larsson M, Nilsson J, et al. Frequent low-level mutations of protein kinase D2 in angiolipoma. J Pathol. 2017;241(5):578-582.
- Ly JQ, Sanders TG, SanDiego JW. Hemangioma of the triceps muscle. Am J Roentgenol. 2003;181:544.
- Mitsionis G, Pakos E, Kosta P, Batistatou A, Beris A. Intramuscular hemangioma of the foot: a case report and review of the literature. Foot Ankle Surg. 2010;16:e27-e29.
- Mitty HA, Kleiger B. Partial embolization of large peripheral hemangioma for pain controls. Radiology. 1978;127:671-672.
- Cohen AJ, Youkey JR, Clagett GP, Huggins M, Nadalo L, d’Avis JC. Intramuscular hemangioma. JAMA. 1983;249(19):2680-2682.
|
|
|
|
|
|
|
Search Google Scholar for
|
|
|
Article Statistics |
|
Priya N, Jayanthi C, Vimal M, Srivani SRare Presentation of Intramuscular Hemangioma: A Case Series.JCR 2024;14:105-108 |
|
Priya N, Jayanthi C, Vimal M, Srivani SRare Presentation of Intramuscular Hemangioma: A Case Series.JCR [serial online] 2024[cited 2025 Dec 18];14:105-108. Available from: http://www.casereports.in/articles/14/4/Rare-Presentation-of-Intramuscular-Hemangioma.html |

|
|
|
|
|