6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa44e02000000a001000001000f00
6go6ckt5b5idvals|175
6go6ckt5b5idcol1|ID
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Rehabilitation of anterior teeth is one of the most frequent and most demanding tasks clinicians still face [1]. While aesthetics, function, and cost are at the core of patient’s motivation, these goals may conflict with the goal of self-preservation [2]. There is growing opinion that recent advances in implantology have all but replaced the fixed partial denture (FPD) as the treatment of choice for restoring a missing tooth. Aesthetic advances in implants allow for the successful and predictable replacement of missing anterior teeth. Such success may contribute to a “rush to implant” mentality and diminish the value of self-preservation for both our patients and the profession [2,3]. Frequently, teeth not only require prosthetic rehabilitation by means of a crown; they often also need restoration of teeth with posts, particularly when large amounts of dental tissue have been lost because of destructive caries and endodontic treatment [1].
This case report presents interdisciplinary treatment planning of a patient with grossly decayed maxillary anterior teeth and missing posterior teeth, except premolars resulted in reduced vertical dimension leading to changes in facial contour. Interdisciplinary treatment planning, knowledge of available restorative materials, sequencing treatment modalities and adequate communication between all the disciplines involved are the key to a successful treatment outcome while pursuing restorative rehabilitation [4,5].
Case Report
A 19-year-old female patient presented with a chief complaint of badly decayed teeth in the upper front region of the mouth and requested for “better looking teeth” [Fig.1,2]. Patient’s extraoral examination revealed reduced lower facial height and decreased visibility of the vermilion border of the upper lip due to poor teeth support. Intraoral examination revealed poor oral hygiene and grossly decayed carious teeth in relation to most of the maxillary teeth and mandibular molars.

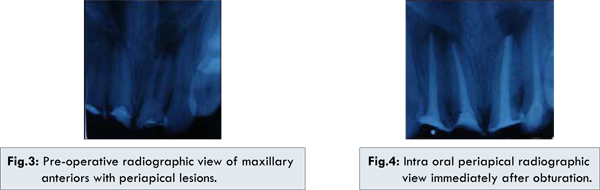
Radiographic examination with intraoral periapical radiograph reveals, periapical lesion in relation to maxillary right and left centrals (11,21) and left lateral incisors (22). Maxillary right central incisor (11) showed an open apex [Fig.3]. The patient underwent a preliminary treatment plan that included professional oral hygiene to restore gingival health, reinforcement of motivation and oral hygiene instructions. Extraction of grossly decayed maxillary and mandibular molars, and maxillary left first premolar was performed at this time. The treatment options discussed with the patient was:
1. Endodontic therapy with surgical crown lengthing followed by post and core and fixed partial dentures’s for anterior teeth and premolars. Replacement of missing posterior teeth with flexible RPD.
2. Extraction of grossly decayed teeth and replacement with implants and fixed partial dentures.
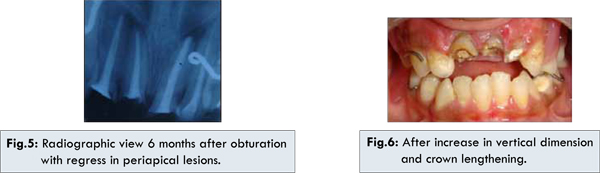
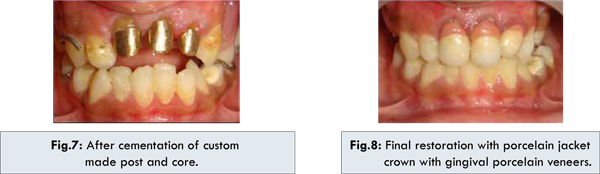
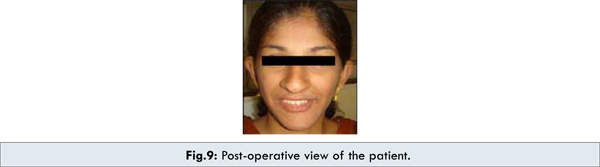
Patient preferred to retain her natural root system and opted for first treatment modality. Endodontic treatment was planned for maxillary central and lateral incisors (11,21,12,22). A thorough biomechanical preparation was done and intracanal medication was placed with calcium hydroxide powder mixed with saline for maxillary central (11,21) and lateral incisors (12,22). Patient recalled at two weeks interval for a month for change of dressing. Custom made rolled cone technique of obturation was done for right maxillary central incisor (11) with open apex. For maxillary left central incisor (21), right lateral incisor (12) and left lateral incisor (22), lateral condensation method of obturation was done [Fig.4]. Following endodontic treatment temporary access restoration was done. Patient was re-evaluated after a period for assessing periapical status of maxillary central (11,21) and lateral incisors (12,22). On radiographic evaluation after 6 months, the periapical lesion showed regress in size in relation to maxillary central incisors (11, 21) and right lateral incisor (12) [Fig.5]. Simultaneously with endodontic treatment, the patients missing posterior teeth were replaced with transient RPD’s which also facilitated restoration of lost vertical dimension. After endodontic treatment an apically repositioned flap with osseous reconturing was done in relation to maxillary anterior teeth to increase the crown length in order to maintain the biologic width [Fig.6].
After allowing proper healing of the gingiva, custom made gold post and core of maxillary centrals (11,21) and left maxillary lateral incisor (22) was fabricated and cemented in position [Fig.7]. Porcelain fused metal crowns were fabricated in relation to maxillary centrals (11,21) and left maxillary lateral (22). Transient RPD’s were replaced with flexible RPD’s. Veneering was done to illusion the increased crown length in relation to incisors [Fig.8,9].
Discussion
The goal of any dental therapy is to facilitate the re-adaptation to a healthy situation that is momentarily damaged. The treatment planning process in dentistry usually begins with an assessment of biological aspects of a patient’s dental problem, which include patient’s susceptibility to caries, periodontal health, endodontic needs and general oral health. Once biological health was addressed, then the restorations of resulting defects were considered and finally aesthetics would be addressed to provide a pleasing appearance of the teeth [4].
This article emphasizes the importance of case selection, interdisciplinary treatment planning and the role of nonsurgical endodontic treatment in preserving strategic teeth. Properly performed, endodontic treatment is the cornerstone of restorative and reconstructive dentistry. Naturally retained root will be recognized as the ultimate dental implant [6,7]. In situations associated with missing posterior teeth, the possibility of developing the pain in temporo-mandibular joint or muscles is highly increased, and the masticatory function is compromised. Thus the patient needs to return to a healthy functional condition prior to any rehabilitation therapy [4].
A provisional removable partial prosthesis momentarily helps to establish the most suitable vertical dimension of occlusion to which the patient can adapt, and does not cause muscle or joint problems. It serves as a guide to the need for correction of pre-existing condition such as collapsed vertical dimension and also helps the patient to relive anxiety about the loss of good facial appearance. In this way a provisional prosthesis fulfils many functions, the most important are the elimination and avoidance of pain and the return to the state of comfort and reasonable function [8]. In this case, the patient received a provisional prosthesis to recover the natural vertical dimension of occlusion, creating the necessary space for aesthetic restorations and making possible a comfortable and functional situation.
Technical restorative procedures require a well defined preparation margins to allow for optimal control of the marginal fit of a reconstruction and optimal access for daily plaque control. Further more, sufficient length of clinical crown is required for optimal retention for the planned reconstruction. So, surgical crown lengthening procedures were performed with apically repositioned flap procedure and osteoplasty was performed [9,10]. The positioning of the alveolar crest at a distance of 3 mm from the future reconstruction margin was done to maintain the biologic width [11,12] .
In the present situation custom-made metal posts were fabricated which provided increased retention and distribution of stresses along the root [13]. Finally all the teeth were restored prosthodontically with porcelain jacket crowns with gingival porcelain veneers towards the marginal gingiva for good esthetic results.
Conclusion
The present case reports a multidisciplinary management of maxillary anterior teeth with another opportunity to use the natural root system and prevent the premature sacrifice of a tooth by endodontic therapy, a provisional prosthesis to recover the natural vertical dimension, surgical crown lengthening to maintain stable periodontal tissue levels, custom made post and core for retention and finally prosthetic rehabilitation with porcelain jacket crowns.
The treatment described in this case report is not intended to preclude more definitive treatment to restore the posterior occlusion with osseointegrated implants and fixed prosthesis, but it is presented as a relatively cost-effective option for patients who cannot afford comprehensive multidisciplinary restorative therapy.
References
- Silvestri M, Silvestri E, Passaler L. Periodontal and prosthetic restoration of the anterior maxilla: A case report. Int J Periodontics Restorative Dent. 2006;26:233-237.
- Morris MF, Kirkpatrick TC, Rutledge RE, Schindler WG. Comparison of nonsurgical root canal treatment and single-tooth implants. J Endod. 2009;35:1325-1330.
- Hannahan JP, Eleazer PD. Comparison of success of implants versus endodontically treated teeth. J Endod. 2008;34:1302-1305.
- Spear FM, Kokich VG, Mathews DP. Interdisciplinary management of anterior dental esthetics. J Am Dent Association. 2006;137:160-169.
- Nam J, Raigrodski AJ, Heindl H. Utilization of multiple restorative materials in full-mouth rehabilitation: A clinical report. J Esthet Restor Dent. 2008;20:251-265.
- Ruddle CJ. Nonsurgical endodontic retreatment. J Calif Dent Assoc. 2004;12:474-484.
- Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JYK. Clinical complications with implants and implant prostheses. J Prosth Dent. 2003;90:121-132.
- Soares CJ, Pizi ECG, Fonseca RB, et al. Direct restoration of worn maxillary anterior teeth with a combination of composite resin materials: A case report. J Esthet Restor Dent. 2005;17:85-92.
- Martins TM, Fernandes LA, Mestrener SR, Saito CTMH, NÓBREGA, Fernando Josà de Oliveira et al. Apically positioned flap: reestablishment of esthetics and integrity of the dentogingival unit. Perspect Oral Sci. 2010;2:43-47.
- Bragger U, Lauchenauer D and Lang NP. Surgical lengthening of the clinical crown. J Clin Periodontol. 1992;19:58-63.
- Carranza FA, Rapley JW, Kinder Hake S. Gingival inflammation. Carranza‘s clinical periodontology. 9th ed. 2002. Chap.16. pp. 263-268.
- Planciunas L, Puriene A, Mackeviciene G. Surgical lengthening of the clinical tooth crown. Stomatologija, Baltic Dental and Maxillofacial Journal. 2006;8:88-95.
- Peroz I, Blankenstein F, Lang KP, Naumann M. Restoring endodontically treated teeth with posts and cores- A review. Quint Int. 2005;36:737-746.