Vijay Kumar Kundal, Raksha Kundal1, Mufique Gajdhar, Chetan Sharma, Deepak Agarwal, Atul Meena
From the Department of Paediatric Surgery and Anaesthesia1,
S.M.S. Medical College & associated SPMCHI, Jaipur-302004, India.
Corresponding Author:
Dr. Vijay Kumar Kundal
Email: vijayraksha@yahoo.com
Abstract
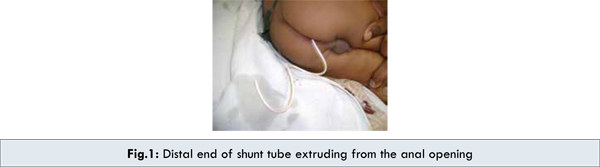
Ventriculoperitoneal (VP) shunt is the standard, time tested surgical procedure for the management of hydrocephalus. Complications associated with VP shunt remain to be persistent problem in clinical setting. However, trans-anal extrusion of VP shunt is rare but well known entity. We are reporting one such case in a six year old male child.
|
6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff248d02000000b301000001000f00 6go6ckt5b5idvals|183 6go6ckt5b5idcol1|ID 6go6ckt5b5|2000F757Tab_Articles|Fulltext Introduction
Ventriculoperitoneal (VP) shunt is one of the commonly performed procedures for the management of hydrocephalus [1]. Although shunts have decreased the mortality and morbidity associated with hydrocephalus, they are still associated with many potentially avoidable complications. The common complications of VP shunt surgery are infection of shunt, blockage and disconnection, migration of shunt tube, shunt failure, bowel perforation, cerebrospinal fluid (CSF) pseudocyst, inguinal hernia and hydrocele. The incidence of abdominal complication reported in the literature is 10-30% [2]. Extrusion of distal end of VP shunt through anal opening is rare and a lesser known complication [3]. We are reporting one such case of transanal extrusion of the distal end of the VP shunt.
Case Report
A six year old male child admitted to us with complaints of extrusion of shunt tube through anal opening during defecation [Fig.1]. There was no history of fever, vomiting or headache. Patient had right VP shunt surgery done for congenital hydrocephalus at the age of 3 months. Clear CSF was seen coming out from tip of extruded shunt tube. General physical examination, systemic examination and digital rectal examination were unremarkable. Complete blood count was within normal range. On X-ray abdomen and pelvis, there was no evidence of pneumoperitoneum and distal end of shunt tube was seen coming out through anal opening [Fig.2]. CSF study from distal extruded shunt tube revealed infection but CSF from lumbar puncture was normal. Patient was kept nil per oral for 72 hours and treated with intravenous antibiotics and distal end was cut after pulling the VP shunt from anal opening and rest of shunt assembly was removed by neck incision. VP shunt revision was done on left side after 1 week. Patient had an uneventful 18 months follow up.

Discussion
Ventriculoperitoneal (VP) shunt represents a classical, universally accepted and commonly used surgical procedure for the management of hydrocephalus [1]. VP shunt diverts the CSF from dilated ventricular system to the peritoneal cavity for fluid absorption. Complications associated with VP shunt are numerous and can be fatal. VP shunt complications are classified as mechanical, infective and functional. These mechanical complications are related to distal peritoneal end of VP shunt and include migration into bowel lumen, intrapleural space, heart, urinary bladder, scrotum, umbilicus, inguinal hernia and other regions [4-8]. Cases of extrusion of the distal shunt catheter through healed abdominal incisions have also been reported [9]. A case of intracardaic migration of distal end of VP shunt has also been reported in the literature [10]. Functional complications include either increased or decreased drainage of CSF.
Intestinal perforation and anal extrusion of a distal VP shunt is an unusual complication. Large intestine is considered the most frequent site of perforation due to VP shunt with an incidence of 0.1-0.7% [11]. The first case of anal extrusion of distal VP shunt was reported by Wilson and Bertrand in 1966 [12]. Since then more than 100 such cases have reported in the literature, predominantly in children. Most of these bowel perforations have asymptomatic course and are diagnosed only after the trans-anal shunt extrusion. Only a small proportion of children have clinical manifestations. Children with meningitis, encephalitis or ventriculitis due to E.coli or other gram negative coliform bacteria should be considered to have an undiagnosed asymptomatic bowel perforation due to VP shunt [13,14].
The exact basis of VP shunt related bowel perforation has not been fully defined. Various proposed mechanisms include foreign body reaction because of silicon tubing of VP shunt, pressure necrosis, and weak bowel musculature. Local inflammation and resulting fibrosis, adherence of shunt tube and continuous water hammer effect of CSF pulsations can erode the intestinal wall. Once in bowel lumen, shunt tube is driven downward and forward by peristaltic waves. Poor host immunity, surgical technique and long shunt tube in peritoneal cavity also contributes to shunt extrusion.
The management of these cases most importantly involves early diagnosis of bowel perforation. X-ray following injection of contrast medium into shunt tubing, can give a clue to the diagnosis. The treatment of these cases involves shunt removal, intravenous antibiotics and re-insertion of shunt at an appropriate time or external ventricular drainage. In case of anal extrusion, distal shunt tube should be divided after traction at an anal verge and remaining shunt assembly should be removed by neck incision. After removal of VP shunt, intestinal perforation heals spontaneously. Emergency laparotomy in required only in cases presenting with features of peritonitis.
In our case, only presentation was spontaneous protrusion of shunt tube from anal opening. Whole of shunt assembly was removed; peritoneal end of shunt tube was divided after traction, as contaminated tube should not be allowed to be in contact with the peritoneum or the shunt tract [15]. It is done to lower the theoretical risk of infection. Revised shunt surgery was done after one week as CSF analysis was normal and patient was clinically asymptomatic.
In conclusion, this case reaffirms the need of close follow up of patients with VP shunts for timely detection and management of potentially fatal complications.
References
- Lifshutz JI, Jonson WD. History of hydrocephalus and its treatments. Neurosurg Focus. 2001;11:E1.
- Bryant MS, Bremer AM. Abdominal complications of ventriculoperitoneal shunts. Case reports and review of literature. Am Surg. 1988;54:50-55.
- Akcora B, Serarslan Y, Sangun O. Bowel perforation and transanal protrusion of a ventriculo-peritoneal shunt shunt catheter. Pediatr Neurosurg. 2006;42:129-131.
- Akyüz M, Ucar T, Göksu E. A thoracic complication of ventriculoperitoneal shunt: symptomatic hydrothorax from intrathoracic migration of a ventriculoperitoneal shunt catheter. Br J Neurosurg. 2004;18:171-173.
- Imamura H, Nomura M. Migration of ventriculoperitoneal shunt into the heart- case report. Neurol Med Chir (Tokyo). 2002;42:181-183.
- Eser O, Dogru O, Aslan A, Kundak A. Umbilical perforation: an unusual complication of a ventriculo-peritoneal shunt. Childs Nerv Syst. 2006;22:1509-1510.
- Zhou F, Chen G, Yhang J. Bowel perforation secondary to ventriculoperitoneal shunt: case report and clinical analysis. J Int Med Res. 2007;35:926-929.
- Ramana Murthy KV, Jayaram Reddy S, Prasad DV. Perforation of the distal end of the ventriculoperitoneal shunt into the bladder with calculus formation. Pediatr Neurosurg. 2009;45:53-55.
- Desousa AL, Worth RM. Extrusion of peritoneal catheter through abdominal incision: report of a rare complication of ventriculoperitoneal shunt. J Neurosurg. 1979;5:504-506.
- Kim BJ, Cha SH, Park DJ, Song GS, Choi CH, Lee YW. A case of intracardiac migration of distal ventriculoperitoneal (V-P) shunt catheter. J Korean Neurosurg Soc. 2000;29:270-273.
- Sathyanarayana S, Wylen EL, Baskaya MK, Nanda A. Spontaneous bowel perforation after ventriculoperitoneal shunt surgery: case report and a review of 45 cases. Surg Neurol. 2000;54:388-396.
- Wilson CB, Bertrand V. Perforation of bowel complicating peritoneal shunt for hydrocephalus: report of two cases. Am Surg. 1966;32:601-603.
- Sharma BS, Kak VK. Multiple subdural abscesses following colonic perforation- a rare complication of a ventriculoperitoneal shunt. Pediatr Radiol. 1988;18:407-408.
- Longstreth G, Buckwalter N. Sterile cerebrospinal fluid ascites and chronic peritonitis. N Engl J Med. 2001;345:297-298.
- Agarwal M, Adhana R, Namdev H, Yadav YR, Agrawal T. Transoral extrusion of the ventriculoperitoneal shunt: A case report and review of literature. Journal of Pediatric Neuroscience. 2011;6:149-151.
|