6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffa4cb02000000c601000001000200
6go6ckt5b5idvals|191
6go6ckt5b5idcol1|ID
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Chronic pyelonephritis presenting as retroperitoneal hemorrhage is a very rare complication and to the best of our knowledge there is only one reported case of acute retroperitoneal hemorrhage complicating a Xanthogranulomatous pyelonephritis [1]. We here present an atypical case of Xanthogranulomatous pyelonephritis presenting with acute retroperitoneal haemorrhage ending up with nephrectomy.
Case Report
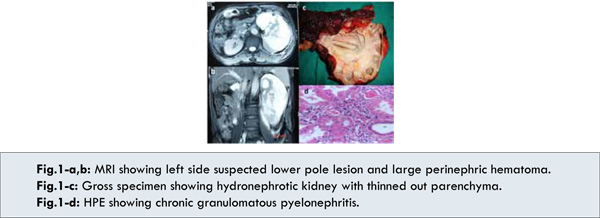
A 60 year old male patient presented with complaint of left side flank pain, intermittent fever and weakness for past 15 days. Pain was continuous as dull ache most of the times with intermittent exacerbations of pain radiating to back and left iliac fossa. Pain used to increase on activity and use to subside on analgesics. Pain was associated with low to moderate grade intermittent fever mostly at times of pain and subsiding on symptomatic treatment. Patient also felt weakness and around 10% weight loss in last two weeks but had no complaint of any urinary symptom or associated abdominal lump. Patient was known diabetic, irregularly treated with oral hypoglycemic agents. Patient had no other comorbidity, no history of trauma or surgery and no significant past personal or family history. Patient was referred to out institute with finding of left perinephric collection on ultrasonography. Examination revealed vague fullness and tenderness of left lumber and renal angle with no obvious lump. Patient was anaemic (Hb. 9 gm %) with raised WBC count (13500/mm3) & serum creatinine of 2.6 mg %. Urine culture was positive for Klebsiella hence patient was started on intravenous antibiotics and supportive care. MRI abdomen revealed hydronephrotic left kidney with ill defined suspected mass in lower pole suggesting large left sided perinephric hematoma reaching upto left iliac fossa [Fig.1a,b]. Patient was planned for exploration for suspected diagnosis of Angiomyolipoma with retroperitoneal haemorrhage. On exploration patient had large retroperitoneal hematoma surrounding left kidney and reaching upto iliac fossa. After evacuation of clots, kidney was found to be hydronephrotic with thinned out parenchyma with some palpable thickening at lower pole hence left nephrectomy was performed [Fig.1c]. Postoperatively, patient recovered well with serum creatinine 1.4 mg% at discharge. Histopathological examination (HPE) revealed Chronic Granulomatous Pyelonephritis with dilated vascular channels in some areas but no evidence of any neoplasia [Fig.1d].
Discussion
Spontaneous retroperitoneal bleeding is a distinctive clinical entity that can present in the absence of specific underlying pathology or trauma [2]. Spontaneous retroperitoneal hemorrhage is rare and most commonly caused by anticoagulant therapy, bleeding abnormalities or hemodialysis [3]. Diagnosis is often delayed because of the lack of specific presenting symptoms. Patients may present with back, lower abdominal or groin discomfort and swelling, which may progress to haemodynamic instability, collapse and a fall in hemoglobin, depending on the severity of the haemorrhage.
Xanthogranulomatous pyelonephritis is a rare variety of chronic pyelonephritis known to give pseudotumor appearance on imaging and final differentiation is by histopathology after nephrectomy in most of cases [4]. Our case matches the findings as hydronephrotic kidney in diabetic male in sixth decade and doubtful lesion in lower pole and ended up with nephrectomy. Although the final histopathology was not characteristic of XGP, lacking classical lipid laden foamy macrophages. Experience with such cases adds up one more very rare but possible way of presentation of chronic granulomatous pyelonephritis.
Probable explanation to the condition in this case could be, the neovascularization associated with chronic inflammatory process with poor coagulopathy associated with associated chronic renal failure. Although these points remain a hypothesis without any further confirmation.
Conclusion
Xanthogranulomatous Pyelonephritis remains a difficult condition to diagnose preoperatively and most of patients end up in nephrectomy as condition cannot be differentiated from malignancy. Acute retroperitoneal hemorrhage in this setting is very rare occurrence. Further research is required to evaluate actual reasons for this occurrence.
References
- Canale S, Deux JF, De la Taille A, Bouanane M, Luciani A, Rahmouni A. Acute retroperitoneal hemorrhage complicating a xanthogranulomatous pyelonephritis. Eur Radiol. 2007;17:1128-1129.
- Pode D, Caine M. Spontaneous retroperitoneal hemorrhage. J Urol. 1992;147:311-318.
- Bhasin HK, Dana CL. Spontaneous retroperitoneal hemorrhage in chronically hemodialyzed patients. Nephron. 1978;22:322-327.
- Eastham J, Ahlering T, Skinner E. Xanthogranulomatous pyelonephritis: clinical findings and surgical considerations. Urology. 1994;43:295-299.