6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ff745003000000ea01000001000f00
6go6ckt5b5idvals|211
6go6ckt5b5idcol1|ID
6go6ckt5b5|2000F757Tab_Articles|Fulltext
Introduction
Tuberculosis is a common disease of tropical countries. Tuberculosis of bowel distal to ileocaecal valve is rare and rarely considered as a differential diagnosis of proctocolic disorder [1]. Tuberculosis of gastrointestinal tract may be of primary or secondary to the primary focus elsewhere [2]. Primary tuberculosis is caused by bovine tubercle bacilli through intake of infected milk. Suppuration and anal fistulae are the most common anorectal tuberculous lesions seen in clinical practice. Sometimes patients of anal tuberculosis may simulate carcinoma clinically. This group of patients usually present with anal mass, ulcer, non-healing fistula, anal pain or bleeding per rectum. In this article, we report a case of anorectal tuberculosis which was clinically suspected as carcinoma of anorectal region.
Case Report
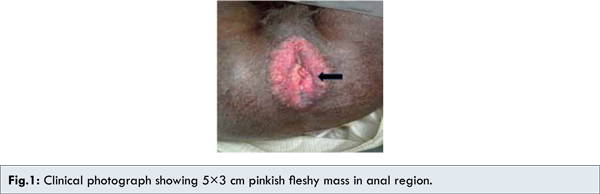
A 58 year old male patient presented with a rapidly increasing mass around anus for last 8 months and history of gradual loss of weight for last one year. There is no history of prolonged fever or change in bowel habits.Physical examination showed that the patient had poor general health and examination of local area showed pinkish fleshy, firm mass which was 5×3 cm in diameter with nodular and ulcerated surface along with indurated base around anus [Fig.1].
Complete hemogram showed increased ESR. Other investigations of blood were unremarkable. The patient was serologically negative for HIV. As the lesion was non healing and clinically simulating a malignant lesion, punch biopsy was taken. Microscopic examination revealed multiple caseating granulomata consisting of epithelioid cells and numerous Langhans type of giant cells with infiltration of chronic inflammatory cells and histiocytes around a central caseating area [Fig.2]. The section was stained by Ziehl - Nielsen method and acid fast bacilli were identified [Fig.3].
Subsequently, the search for the primary focus was started and X ray chest (PA view) showed opacities in upper and mid zones of right lung suggestive of pulmonary tuberculosis. Acid fast bacilli were detected in sputum examination. However, mantoux test was negative. A diagnosis of anal tuberculosis of lupoid type secondary to pulmonary tuberculosis was made.
Discussion
Clinical presentation of anal tuberculosis displays a wide range of symptoms of which anal mass, ulcer, non-healing fistula, pain and bleeding per rectum are important. The differential diagnoses for our case were carcinoma of anal canal and Crohn’s disease.
The lesions of anal carcinoma have rolled out everted edges with central ulceration. Carcinoma of anal canal was excluded by histopathology in this case. Crohn’s disease is seen mostly in teenagers and young individuals, while anorectal tuberculosis is seen in patients older than 30 years [3]. Moreover, the granuloma in Crohn’s disease is a noncaseating. Presence of caseating granuloma and acid fast bacilli excluded Crohn’s disease in this case.
Anorectal tuberculosis is classified in four types, as ulcerative, verrucous, lupoid and miliary [4]. Ulcerative form is the most common type and usually secondary to a focus in lungs or intestine. Verrucous tuberculosis is characterized by warty vegetation. These lesions slowly increase in size. Mycobacterium bovis is the causative organism. Lupoid tuberculosis is secondary to a tuberculous condition elsewhere in the body. It begins as a small, soft, round nodule which is reddish brown in color. Gradually a clean-cut ulcer, with an indurated base and showing a mucopurulent discharge, develops in the center of the nodule. Miliary lesions of the anus occur as part of disseminated tuberculosis, involving many organs [5]. It is speculated that tuberculous anal lesions are caused by dissemination from the pulmonary focus via hematogenous and lymphogenous spread in few patients, while in others the lesion may be present in the gastrointestinal tract and rectum [6]. In our case, tuberculous lesion in anus occurred as a secondary involvement by hematogenous spread from the primary focus in the lungs.
While the incidence of patients with extra pulmonary tuberculosis has increased in the last few years (about 5% of all cases) displaying a wide spectrum of its clinical manifestations, the anal localization still is rare (0.7%) according to available published data [7]. Three cases, encountered over a period of 10 years, were reported from Prince of Wales Hospital in Hong Kong [1]. In one report from India, 19 out of 122 cases of perianal fistula were diagnosed as tuberculosis.
Conclusion
It can be concluded that tuberculous origin must be considered in the differential diagnoses of unknown anal nodular and ulcerated lesions especially in recurrent ones.
References
- Chung CC, Choi CL, Kwok SP, Leung KL, Lau WY, Li AK. Anal and perineal tuberculosis: a report of three cases in 10 years. J R Coll Surg Edinb. 1997;42:189-190.
- Iwase A, Shiota S, Nakaya Y, Sakamoto K, Aoki S, Matsuoka R, Nagayama T. An autopsy case of seven tuberculosis associated with anal fistula and intestinal perforation. Kekkaku.1997;72:515-518.
- Logan D. Anorectal tuberculosis. Proc Roy Soc Med. 1969;62:1227-1230.
- Nepomuceno OR, Grady JFO, Eisenberg SW, Bacon HE. Tuberculosis of the anal canal: report of a case. Dis Col & Rec. 1971;14:313-316.
- Altmoz H, Kose E, Kula O, Keser B, Karagoz T. Pulmonary Tuberculosis Complicated by Anal Tuberculosis. Turk Resp Jour. 2003;4:142-143.
- Onizuka O, Kawano M, Aso S. A case of tuberculous anal fistulae complicated by pulmonary tuberculosis. Kekkaku.1994;69:689-692.
- Alvarez Conde JL, Gutierrez Alonso VM, Del Riego Tomas J, Garcia Martinez I, Arizcun Sanchez-Morate A, Vaquero Puerta C. Perineal ulcers of tubercular origin. A report of 3 new cases. Rev Esp Enferm Dig. 1992;81:46-48.