6go6ckt5b8|3000F7576AC3|Tab_Articles|Fulltext|0xf1ffe4173a0000005b07000001000500
Introduction
Arachnoid granulations are structures filled with cerebrospinal fluid (CSF) that extend into the venous sinuses through openings in the dura mater and allow the drainage of CSF from subarachnoid space into the venous system, size of these granulations varies from a few millimetres to more than 1?cm when called as giant arachnoid granulations [
1]. These granulations may grow to fill and dilate the dural sinuses or expand the inner table of the skull, the presence of pre-existing arachnoid granulations facilitates the brain herniation into the dural venous sinus (DVS) or adjacent calvarium which is thought to arise spontaneously or as a result of increased intracranial pressure [
2]. Brain herniations into arachnoid granulations (BHAGs) are rare findings of undetermined etiology and significance and are incidentally recognised when patients undergo imaging for some other reason. Battal et al. reported that prevalence of BHAGs is 0.32%. The most common location of BHAGs are the occipital squama and transverse sinus [
3,
4]. Posterior brain region involving cerebellar hemispheres, occipital lobes herniate more followed by inferior temporal gyrus, occipitotemporal gyrus, parietal cortex and superior frontal gyrus [
5,
6]. Usually they are asymptomatic but can be symptomatic when large enough to cause sinus occlusion. We report a rare case presenting in epilepsy clinic for refractory seizures and found to have brain herniation into arachnoid granulation on neuroimaging.
Case Report
A 17-year-old male patient presented to us with a history of multiple episodes of abnormal posturing of the body and unresponsiveness for the last 20 days, after a family conflict. These episodes persist for a variable duration of 10 minutes to 2-3 hours, semiology being episodes of abdominal and chest discomfort, hyperventilation followed by variable posturing of both upper limbs, flexion of both lower limbs at hip and knee joint, tight closure of eyes, and opisthotonos posturing without any urinary and fecal incontinence, tongue bite, the patient didn’t suffer injury in any of these episodes, there was no period of confusion or amnesia associated with the event, no history of any automatism, hallucinations, or other type seizures. Family history was not contributary. Birth and developmental history were normal with febrile seizures (3 episodes) before the 3 years of age that subsided without need of any anti-epileptics.
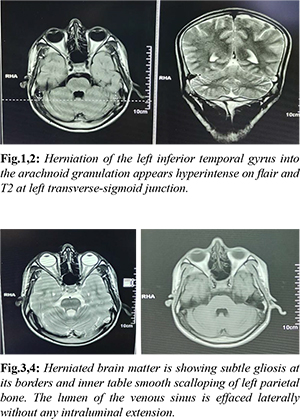
His general and neurological examination was normal. As patient was not responding to two anti-epileptic drugs and with bizarre event semiology, he was subjected to long term video EEG for 3 days which captured five events, when analysed showed clinical events of non-stereotypical episodes of pelvic thrusting, opisthotonos posturing, side-to-side movement of the body, forceful eye closure and bizarre behaviour of act of strangulation during the events. These events increased in presence of family persons. On EEG correlation, there were no ictal epileptiform discharges during the events confirming that the events were psychogenic non-epileptic seizures (PNES). Background rhythm was sinusoidal alpha of 8-9 Hz with preserved reactivity to eye opening and closure. There were no interictal epileptiform discharges noted. Neuroimaging (MRI Brain) showed herniation of the left inferior temporal gyrus into the arachnoid granulations of the left transverse-sigmoid junction, and associated minimal herniation of adjacent CSF spaces along with brain parenchyma. The herniated brain matter showed subtle gliosis at its borders. CT correlation showed smooth scalloping of the inner table of the adjacent left parietal bone, the lumen of the sinus effaced laterally without any intraluminal extension. The clinico-EEG correlate and the imaging findings confirmed the case of psychogenic non-epileptic seizures (PNES) with incidental finding of brain herniation into arachnoid granulation (BHAG). Patient was given counselling by psychiatric unit and anti-epileptics were slowly tapered and withdrawn. Patient has markedly improved after counselling.
Discussion
Arachnoid granulations (AG) were first described by Antonio Pacchioni in 1705. These are arachnoid extension into sinuses. Arachnoid granulations can enlarge with age or in response to an increase in cerebrospinal fluid pressure and they can be found anywhere in the dural venous sinuses and are macroscopically visible. Most of BHAGs are asymptomatic incidental findings as occurred in our case, but a part of them can potentially be linked to particular symptoms probably due to eloquent brain tissue found in the herniation. Their etiology is not completely understood and many theories are associated with it. Symptoms can occur as a result of venous hypertension secondary to partial sinus occlusion [
7]. Increased intracranial pressure causes brain parenchyma to herniate into arachnoid granulations or it sometimes herniate spontaneously or as a result of increased intracranial pressure, also confirmed by Battal et al. [
8].
Benign intracranial venous hypertension is another clinical phenotype reported with giant arachnoid granulation and daily acetazolamide in 750 mg dosage reduces the symptoms effectively [9]. AG are most reliably seen in FLAIR with totally different CSF intensity (not attenuated) in 100% cases. Flair hyperintensity of CSF could be due to pulsation artifacts from the adjacent sinus. The closest differentials are thrombosis of dural sinuses and neoplasia which can be differentiated by their unique characteristics of involving more extensively and contrast enhancement and diffusion restriction feature, shape respectively. Brain parenchyma herniations into the calvarium are recently described rare controversial entity and encountered more frequently in posterior inferior parts of the intracranial cavity. Brain herniations into AG are most commonly located in the occipital squama, followed by transverse sinus, lateral lacuna of the superior sagittal sinus, and straight sinus. Cerebellar tissue is the most frequent found in these herniations but cerebral tissue can also herniate. Brain parenchyma herniations affect more women than men [5]. Complicated AG result from strangulation of herniated tissue as a result of narrow neck which causes infarction of the herniated parenchyma which can result in brain dysfunction and seizures. Our patient though had apparent seizure like events which were confirmed to be PNES on video EEG and it was mere incidental association of BAGH and PNES. The rarity and unique presentation bring this case for highlight.
Conclusion
This case is presented for its rarity and unique association of BAGH with PNES. It’s potential relation with above mentioned symptoms in some of the patients makes them an important entity to be identified. It is important to recognize both arachnoid granulations and BHAGs correctly and avoid confusing them with normal filling defects of dural sinuses such as septae or fat, or with pathological conditions including sinus thrombosis, malignancy or encephalocele. The author tried to bring this less recognised entity ang describe the facts related to it.
Contributors: AD: manuscript editing, critical inputs into the manuscript; PVK: manuscript drafting, literature search, patient management. PVK will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Trimble CR, Harnsberger HR, Castillo M, Brant-Zawadzki M, Osborn AG. “Giant” arachnoid granulations just like CSF?: NOT!! American Journal of Neuroradiology. 2010;31(9):1724-1728.
- Battal B, Hamcan S, Akgun V, Sari S, Karaman B. Brain herniation with surrounding CSF into the skull or encepholecele? Journal of Neuroradiology. 2015;42:187-188.
- Battal B, Hamcan S, Akgun V, Sari S, Oz O, Tasar M, et al. Brain herniations into the dural venous sinus or calvarium: MRI findings, possible causes and clinical significance. Eur Radiol. 2016;26:1723-1731.
- Liebo GB, Lane JJ, Van Gompel JJ, Eckel LJ, Schwartz KM, Lehman VT. Brain herniation into arachnoid granulations: clinical and neuroimaging features. J Neuroimaging. 2016;26:592-598.
- Malekzadehlashkariani S, Wanke I, Rüfenacht DA, Millán DS. Brain herniations into arachnoid granulations: about 68 cases in 38 patients and review of the literature. Neuroradiology. 2016;58:443-457.
- Kosnik EJ, Meagher JN, Quenemoen LR. Parietal intradiploic encephalocele. J Neurosurg. 1976;44:617-619.
- Kan P, Stevens EA, Couldwell WT. Incidental giant arachnoid granulation. AJNR Am J Neuroradiol. 2006;27(7):1491-1492.
- Battal B., Hamcan S, Akgun V, Sari S, Oz O, Tasar M, et al. Brain herniations into the dural venous sinus or calvarium: MRI findings, possible causes and clinical significance. European Radiology. 2016;26(6):1723-1731.
- De Keyzer B, Bamps S, Van Calenbergh F, Demaerel P, Wilms G. Giant arachnoid granulations mimicking pathology. A report of three cases. Neuroradiol J. 2014;27(3):316-321.