Introduction
Epididymal rhabdomyosarcoma is an exceptionally rare mesenchymal tumor, and its occurrence in young adults is an even rarer phenomenon. Typically, this aggressive malignancy primarily afflicts children and adolescents, often presenting as a painless scrotal mass. The scarcity of documented cases in young adults underscores the significance of reporting and analyzing such instances to expand our understanding of this malignancy.
In this case report, we present the clinical journey of an 18-year-old male who came to medical attention with a painless left scrotal mass that had gradually developed over a span of three months. Through this report, we aim to shed light on the challenges posed by this uncommon presentation, highlight the importance of early detection, and underscore the potential for successful treatment approaches in managing epididymal rhabdomyosarcoma in young adults. The comprehensive assessment and management of such cases are vital for optimizing clinical outcomes and advancing our knowledge of this unusual manifestation.
Case Report
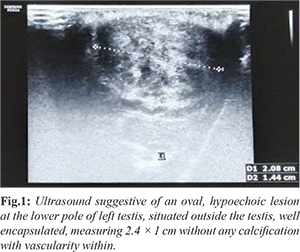
We present the case of an 18-year-old patient who presented with a painless scrotal mass that had been progressively evolving over a three-month period. Upon examination, the mass measured 2 × 2 cm, was firm, non-tender, and palpable separately from the testis. Clinical examinations of lymph nodes and the abdomen yielded normal findings. Subsequently, routine abdomen and pelvis imaging, along with scrotal sonography, indicated the presence of an encapsulated mass on the left side, situated outside the testis, displaying vascularity within but devoid of calcifications [Fig.1]. This presentation raised suspicion of an adenomatoid tumor of the epididymis or leiomyoma.
Serum alpha-fetoprotein (AFP) levels were found to be 2.5 ng/mL, and beta-human chorionic gonadotropin (HCG) levels were less than 0.13 ng/mL, both within normal ranges. The patient then underwent excision of the para-testicular mass, and histopathological analysis confirmed the diagnosis of spindle cell rhabdomyosarcoma [Fig.2]. Immunohistochemistry further revealed that the tumor cells were diffusely positive for desmin, myogenin, and MYOD1, while being negative for AE1/AE3 and CD31 [Fig.3-7]. Subsequently, a left high inguinal orchidectomy was performed, along with excision of the scrotal scar. Histopathological examination revealed a vaguely nodular area near the lower pole of the testis, which displayed residual neoplasm composed of fusiform, elongated/spindle to ovoid cells arranged haphazardly, indicative of sclerosing rhabdomyosarcoma.
The patient received a total of 23 cycles of radiotherapy coupled with 12 cycles of chemotherapy, following a regimen that included Vincristine (2 mg/m2), Dactinomycin (1.6 mg/m2), and Cyclophosphamide (3 gm/m2). Each chemotherapy session was completed within a single day, with a 21-day cycle interval.
Discussion
Rhabdomyosarcoma usually occurs in the extremities. A para-testicular localization is rare; the tumor develops from mesenchymal tissues of the spermatic cord, and epididymis [
1]. There are two frequency peaks found for the development of rhabdomyosarcoma, the first at the age of 4 years and the second at the age of 18 years, as in our case. There is no predilection for race [
2]. Primary tumors of the epididymis and spermatic cord are very rare. Differential diagnoses include testicular torsion, epididymoorchitis, scrotal abscess and, rarely testicular tuberculosis. Embryonal rhabdomyosarcoma is the most frequent malignant tumor of the spermatic cord in children and young adults, but it may also occur in the testis, epididymis and testicular tunica. These tumors tend to spread via the lymphatic system to iliac lymph nodes; nevertheless, spread via the blood stream to the liver and lungs do occur. The clinical presentation of our patient, an 18-year-old male, with a progressively evolving painless scrotal mass, is consistent with reported cases of epididymal rhabdomyosarcoma. The firm, non-tender nature of the mass, separate from the testis, is a characteristic feature often seen in such cases. Synchronous or metachronous involvement of the pelvic lymph nodes. Embryonal rhabdomyosarcoma may occasionally show small groups of anaplastic cells with bizarre nuclei that seem to be associated with a more aggressive clinical course. Recently, a new histologic appearance termed spindle cell rhabdomyosarcoma has been identified in patients with low stage paratesticular primaries. Other variants of rhabdomyosarcoma are alveolar, orphic and pleomorphic.
A testicular ultrasound is routinely performed for a scrotal mass. This imaging modality shows a mass with heterogeneous echogenicity and inguinoscrotal extension in 80% of cases [3]. This allows the nature of the intra-scrotal tissue mass to be determined and specifies the exact topography. Ultrasound is used to establish the differential diagnosis and eliminate diagnoses of simple cyst and varicocele. A thoraco-abdomino-pelvic CT scan allows for any deep invasion of the lymph nodes to be investigated, especially lumbo-aortic and pelvic metastases as well as possible metastases to the liver or lung. Most authors prefer the use of thoraco-abdomino-pelvic CT compared to ultrasound for lymphomas. Magnetic resonance imaging is an efficient imaging modality when using surface coils. The tumor appears homogeneous in T1-weighted images and heterogeneous in T2-weighted images with signal intensity similar to that in a normal testis. The low signal intensity of the tunica albuginea in T2-weighted images allows the visualization of a clear separation of the mass from the testis [4,5]. Serum tumor markers, such as AFP and beta HCG, were within normal limits, which is consistent with previous reports of epididymal rhabdomyosarcoma in young adults. These findings emphasize that relying solely on tumor markers for diagnosis can be misleading in cases of this rare malignancy. Histopathological analysis remains the gold standard for diagnosing rhabdomyosarcoma. Our case, displaying spindle cell rhabdomyosarcoma on histology, aligns with the known pathology of this tumor. Immunohistochemistry further confirmed the diagnosis by demonstrating diffuse positivity for desmin, myogenin, and MYOD1, which are characteristic markers of rhabdomyosarcoma. The treatment of epididymal rhabdomyosarcoma involves a multimodal approach, often including surgical excision, chemotherapy, and radiotherapy. In our case, the patient underwent a left high inguinal orchidectomy followed by an extensive regimen of chemotherapy and radiotherapy. On consideration of the small size of the neoplasm and the absence of metastases in our patient, we opted for watchful waiting, adjuvant therapy and with careful follow-up. The treatment of patients with high grade tumor, or tumors larger than 5 cm and those with metastatic disease will require innovative collaborative studies with multimodality treatments, which have so far been hampered by the rarity of these lesions. The successful clinical improvement observed two months after completing chemotherapy highlights the effectiveness of this comprehensive treatment strategy.
Conclusion
Epididymal rhabdomyosarcoma remains a rare and diagnostically challenging entity, especially when presenting in young adults. This case underscores the importance of considering this malignancy in the differential diagnosis of scrotal masses, even among older age groups, to ensure early detection and appropriate management.
Contributors: AI, IM: manuscript writing, patient management; HM, RV, AS: manuscript editing, patient management; MP, AR, JM: critical inputs into the manuscript. AI will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Masson BJ, Kier R. Sonographic and MR imaging appearances of paratesticular rhabdomyosarcoma. Am J Roentgenol. 1998;171:523-524.
- Wiener ES, Lawrence W, Hay D, Lobe TE, Andrassy R, Donaldson S, et al. Retroperitoneal node biopsy in paratesticular rhabdomyosarcoma. J Ped Surg. 1994; 29:171-178.
- Heyn R, Raney RB, Hays DM, Tefft M, Gehan EA, Webber B, Maurer HM. Late effects of therapy in patients with paratesticular rhabdomyosarcoma. J Clin Oncol. 1992;10:614-623.
- Kasmaoui E, Jira H, Alami M, Ghadouane M, Ameur A, Abbar M. Les rhabdomyosarcomes paratesticulaires: à propos de trois cas. Ann Urol. 2001;35:296-300.
- Bouchikhi AA, Mellas S, Tazi MF, Lahlaidi K, Kharbach Y, Benhayoune K, et al. Embryonic paratesticular rhabdomyosarcoma: a case report. Journal of Medical Case Reports. 2013;7:1-3.