|
Desmond Lim Shi Wei1, Ma Li2, Raju Gangaraju Changal3, Lynette Li San Teo1 Departments of 1Diagnostic Imaging, 2Obstetrics & Gynaecology and 3Pathology, National University Hospital, 5 Lower Kent Ridge Rd, Singapore 119074.
Corresponding Author:
Dr Lynette Li San Teo Email: lynette_ls_teo@nuhs.edu.sg
Abstract
Background: This case illustrates the challenges of clinical assessment of a pregnant patient in the third trimester. Use of non-radiation-based imaging modalities become more critical in the evaluation of the surgical abdomen in pregnant mothers. We discuss the advantages of ultrasound (US) and Magnetic Resonance Imaging (MRI) in the evaluation of a pregnant lady. Case Report: A 29-year-old lady, gravid 2 para 1 at 32 weeks gestational age presented with intermittent right iliac fossa pain. Physical examination revealed poorly localising right sided abdominal tenderness. An US performed showed a large mass in the right iliac fossa but was otherwise non-diagnostic. Subsequently torsion of an ovarian dermoid cyst was diagnosed with unenhanced MRI. Urgent surgery was performed thereafter with good outcome. Conclusion: Unenhanced MRI is now widely available and is increasingly a helpful tool for diagnosis to achieve prompt treatment and symptom relief.
|
Introduction
Ovarian torsion presenting in a third trimester patient is an unusual and if not a rare occurrence with only a handful of reports [ 1- 3]. We report a case diagnosed with Magnetic Resonance Imaging (MRI) and illustrate the uses of MRI in the evaluation of a surgical abdomen in a pregnant patient. The evaluation of a surgical abdomen in a pregnant patient is a diagnostic challenge, often due to anatomical distortion due to the gravid uterus. Ultrasound and MRI are the mainstays in pregnant patients each of them having their own advantages and disadvantages. Ultrasound examination is an easily accessible bedside tool which provides the operator not only the chance for correlation with graded compression of visualized anatomical structures, but also allows for vascular flow assessment. MRI provides superior anatomical localization, opportunistic screening of the fetus and valuable information for pre-operative planning especially due to distorted anatomy from the gravid uterus. MRI evaluation should be considered in equivocal US and clinical examination findings.
Case Report
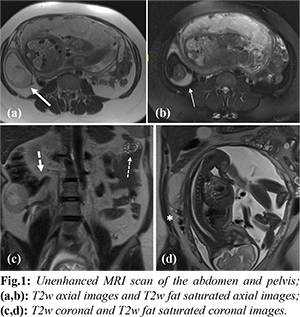
A 29-year-old lady, gravid 2 para 1 at 32 weeks gestational age presented with intermittent right iliac fossa pain. This had lasted for less than a day and was described as excruciating and associated with nausea, vomiting and diarrhoea. Physical examination revealed poorly localizing right sided abdominal tenderness. The gravid uterus was palpable above the umbilicus. She was tender on deep palpation of the right hypochondrium and had rebound tenderness of the right iliac fossa. The patient was otherwise hemodynamically stable and afebrile. Obstetrics assessment in the emergency department revealed that the fetal parameters were normal and the membranes were intact. Laboratory investigations showed mild anemia likely related to pregnancy, the patient’s hemoglobin was 10.3 g/dL (normal range 11.4 - 14.7). Her inflammatory markers were not elevated (total white blood cell count 10.3 g/dL, normal range 3.8 - 10.1). Bedside urine dipstick was normal. An ultrasound showed a large heterogenous mass partially visualized in the right lower abdomen. Internal hyperechoic areas with relative central hypo-echogenicity were noted. It was difficult to visualize the full extent of the mass and its organ of origin due to limited sonographic windows attributed to overlying bowel gas and the gravid uterus. As ultrasound findings were non-diagnostic, an unenhanced MRI of the abdomen and pelvis was performed. The unenhanced MRI images show a right adnexal cystic lesion [Fig.1a, thick white arrow] measuring approximately 5×7 cm. This contained an internal fat-fluid level appearing T1-weighted hyperintense with the non-dependent component showing fat suppression [Fig.1b, thin white arrow]. This indicates layering of internal macroscopic fat and haemorrhage. Clear visualisation of the internal fat component allowed for the diagnosis of a dermoid cyst. The vascular pedicle of the right adnexal lesion was seen in the inferior pole and appeared engorged with a corkscrew appearance (white asterix). The coronal images show the vascular pedicle coursing towards the inferior vena cava, suggesting the right ovarian origin of the lesion [Fig.1c]. Also seen on the coronal images are the normal left ovary (thin dashed arrow) and the normal appendix (thick dashed arrow).
Upon diagnosis the patient underwent a laparoscopic exploration, de-torsion of the right ovary and right cystectomy. Intra-operatively the right ovary contained a dermoid cyst of up to 7 cm and the right ovary was torted 4 times. Upon detorsion, the right ovary appeared viable and was left in situ. Gross examination of the resected specimen showed a cyst containing a ball of hair and sebaceous material. A subcentimeter fragment of bone was found internally. The cyst wall was noted to be haemorrhagic. Microscopic examination showed a mature cystic teratoma [Fig.2] composed of skin with adnexal structures, glial tissue, adipose tissue, thyroid tissue and cartilage among others. No immature tissue components or neuroepithelial tubules were identified. There was no evidence of malignancy. The patient made an uneventful recovery in the ward and was fit for discharge the following day. She went on to have a normal vaginal delivery of her child.
Discussion
In the evaluation of a surgical abdomen in pregnant patients, ovarian torsion is an important differential to consider due to its non-specific clinical presentation and potential for deterioration if left untreated. A case report of ovarian torsion in the third trimester led to preterm delivery of the fetus [ 1]. Rotation of the vascular pedicle results in interruption of ovarian venous drainage before threatening arterial perfusion. Coagulation necrosis eventually ensues which may eventually lead to a nidus for sepsis and eventual morbidity and mortality [ 2]. The incidence of ovarian torsion ranges from 2-15% [ 3, 4]. This is relatively uncommon, and the diagnosis is further confounded due to overlapping symptoms and signs with other more common diagnoses including: cholecystitis, appendicitis and renal colic. In pregnancy, the incidence of ovarian torsion is even more uncommon [3,5]. Prior retrospective studies and case reports noted higher incidence in the 1st trimester likely due to rapidly enlarging physiological cysts [5]. Classical teaching reports ovarian torsion to be commoner on the right than the left, postulated due to limited adnexal movement by the sigmoid colon in pregnancy. Ovarian torsion is often associated with a lead point, due to existing ovarian lesions/tumors, as in our case where the patient had a dermoid cyst of the affected ovary [6]. The evaluation of surgical abdomen in the pregnant patient is limited to non-radiation-based imaging modalities: ultrasound and MRI. Ultrasound (US) allows for accessible bedside examination and can adapt to various positions of the patient which would be convenient in gravid pregnancy if the patient has difficulty lying supine. The ability to correlate with graded compression of the abdomen increases the specificity of the examination. In addition, Doppler imaging provides vital information of vascular flow when evaluating for ovarian torsion. However, sonographic windows may be severely limited by the gravid uterus and gas within overlying bowel loops. Prior studies show the accuracy of US in diagnosing ovarian torsion to range from 75-84% [7,8]. Unilateral ovarian enlargement was found to be most supportive. Other findings included ovarian edema, abnormal adnexal position, absence/decreased blood flow and a whirlpool appearance of the visualized pedicle. A combination of sonographic findings and clinical suspicion is still required for the diagnosis. The use of MRI in the diagnosis of ovarian torsion with equivocal US findings is only recently more employed. Retrospective studies reported this to be within the range of 80-85% [ 9]. Only a handful of case reports demonstrated the diagnosis of ovarian torsion using MRI after equivocal US findings [ 10- 13]. MRI not only allows for better anatomical delineation but also for exclusion of the differential diagnoses. Cross sectional images are also useful for pre-operative planning. The use of MRI is difficult if the patient is unable to lie supine for extended periods of time and limited by its availability. MRI examinations in pregnancy are strictly performed without contrast due to the potential harmful effects of gadolinium contrast on the fetus regardless of trimester [ 14]. As such, enhancement characteristics cannot be evaluated which may provide useful information about relative vascular flow within a lesion in an otherwise normal patient.
Conclusion
Overall, the multidisciplinary care of the patient with quick involvement of Radiology and appropriate escalation of imaging modalities led to the diagnosis and prompt treatment of the patient in this case. In the evaluation of a surgical abdomen in a pregnant patient, MRI should be considered in equivocal US and clinical examination findings.
Contributors: DLSW, ML: manuscript writing, patient management; RGC, LLST: manuscript editing, patient management; LLST will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study. Funding: None; Competing interests: None stated.
References - Koumoutsea EV, Gupta M, Hollingworth A, Gorry Anwen. Ovarian torsion in the third trimester of pregnancy leading to iatrogenic preterm delivery. Case Rep Obstet Gynaecol. 2016;2016:8426270.
- Young R, Cork K. Intermittent ovarian torsion in pregnancy. Clin Pract Cases Emerg Med. 2017:1:108-110.
- Bouguizane S, Bibi H, Farhat Y, Dhifallah S, Darraji F, Hidar S, et al. Les torsions des annexes de l'utérus. Aspects cliniques et thérapeutiques: à propos d'une série de 135 cas [Adnexal torsion: a report of 135 cases]. J Gynecol Obstet Biol Reprod (Paris). 2003;32(6):535-540.
- Huang C, Hong MK, Ding DC. A review of ovary torsion. Tzu Chi Med J. 2017;29:143-147.
- Hasiakos D, Papakonstantinou K, Kontoravdis A, Gogas L, Aravantinos L, Vitoratos N. Adnexal torsion during pregnancy: Report of four cases and review of the literature. J Obstet Gynaecol. 2008;34:683-687.
- Duigenan S, Oliva E, Lee SI. Ovarian torsion: diagnostic features on CT and MRI with pathologic correlation. AJR Am J Roentgenol. 2012;198:122-131.
- Mashiach R, Nir M, Gilad N, Ben-Shitrit G, Meizner I. Sonographic diagnosis of ovarian torsion: accuracy and predictive factors. J Ultrasound Med. 2011;30:1205-1210.
- Feng JL, Zheng J, Lei T, Xu YJ, Pang H, Xie HN. Comparison of ovarian torsion between pregnant and non-pregnant women at reproductive ages: sonographic and pathological findings. Quant Imaging Med Surg. 2020;10:137-147.
- Béranger-Gibert S, Sakly H, Ballester M, Rockall A, Bornes M, Bazot M, et al. Diagnostic value of MR imaging in the diagnosis of adnexal torsion. Radiology. 2016;279:461-470.
- Yildirim H, Ozdinc S. A rare condition in the third trimester of pregnancy: Ovarian torsion. Turk J Emerg Med. 2020;20:42-45.
- Born C. Wirth S, Stäbler A, Reiser M. Diagnosis of adnexal torsion in the third trimester of pregnancy: a case report. Abdom Imaging. 2004;29:123-127.
- Li C, Wang S, Tao X, Hu Y, Li X, Xiao X. Torsion of normal-sized ovary during late pregnancy: A case report and review of the literature. J Obstet Gynaecol. 2018;44:2110-2114.
- Bai W, Xu X, Xie H, Sun C, Che K, Liu M, et al. Adnexal torsion in the third trimester of pregnancy: a case report and diagnostic value of MR imaging. BMC Medical Imaging. 2020;20(1):19.
- Symons SP, Heyn C, Maralani PJ. Magnetic Resonance Imaging exposure during pregnancy. JAMA. 2016;316:2275.
|