Introduction
Left sided gall bladder (LSG) is a rare anomaly encountered by surgeons in clinical practice. LSG is defined as a gallbladder located on the left side of the round ligament or ligamentum teres [
1]. LSG can be associated with situs inversus or without situs inversus. The co-existence of choledochal cyst (CC) with pancreas divisum (PD) is rare with less than 10 cases reported in literature [
2]. Pakkala et al. reported 4 cases of CC with PD in their case series [
3]. Hochstetter’s first described left sided gall bladder in 1886 [
4]. The associated anomalies with left-sided gallbladder include portal vein anomalies, biliary system anomalies, and segment 4 atrophy [
4]. We are reporting a case of left sided gall bladder with coexisting choledochal cyst and pancreas divisum.
Case Report
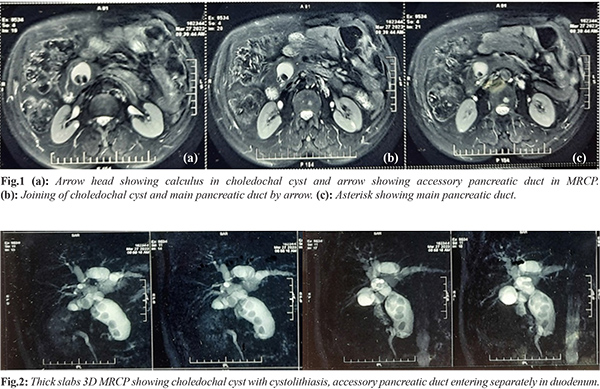
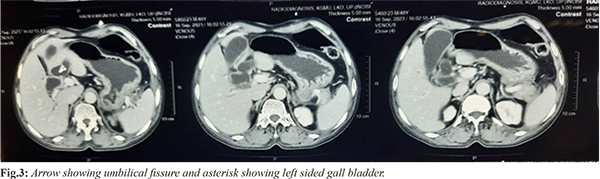
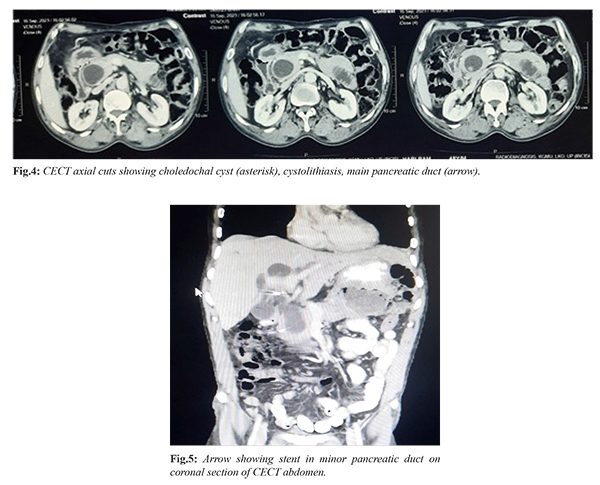
A 48-year male patient came to our department with history of recurrent upper abdominal pain. He was evaluated with ultrasound abdomen, which showed fusiform dilatation of extra-hepatic bile ducts and dilated intra-hepatic biliary radicals and distended gall bladder. Further evaluation was done with complete blood counts, liver function test, renal function test, coagulation profile, serum electrolytes, magnetic resonance cholangiopancreatography (MRCP), which was suggestive of type 4a choledochal cyst with cystolithiasis with pancreas divisum and distended gall bladder [Fig.1,2]. Contrast enhanced computed tomography (CECT) was done showing similar findings [Fig.3,4]. Minor pancreatic duct stenting was done for recurrent acute pancreatitis [Fig.5]. After stenting patient developed severe necrotizing pancreatitis and cholangitis, which was managed conservatively with multiple percutaneous drainage tubes in peripancreatic and left paracolic space and also segment 3 percutaneous transhepatic biliary drainage tube insertion done for cholangitis. After three months of resolution of pancreatitis patient was planned for choledochal cyst excision with intraoperative choledochoscopy with Roux-en-Y hepaticojejunostomy.
Abdomen was entered through upper midline incision, falciform ligament taken down [Fig.6] and gall bladder (GB) was dissected out from GB bed, cystic duct entering CHD on right side, cystic artery ligated and divided, CC was circumferentially dissected but was densely adherent to portal vein and looped, after kocherisation choledochotomy was done, stones extracted and intra-operative choledochoscopy was done for retained stones distally, no pancreatic duct opening identified in CC, proximally no membrane, stenosis, stones, sludge present on choledochoscopy. Distal transection done at waist and proximal transection just below the confluence. Later hepaticojejunostomy done in an interrupted fashion with delayed absorbable suture. In post-operative period patient tolerated orally by day 2, drain was serous and removed on day 5 and discharged on post operative day 7.
Discussion
According to Idu et al. LSG without situs inversus can be of two types. First true LSG where GB is attached to left lobe of liver and second where the gallbladder is on the left side of the round ligament but still on the right lobe of the liver [
5]. In patients with LSG cystic duct can join from right or left side. Nagai et al. found cystic duct joining from right side in 20 patients and 19 from left side of common bile duct in their 41 patients [
6]. In this case it was joining from right side. Pancreas divisum is most common congenital anomaly of pancreas. One of theory of choledochal cyst formation is reflux of pancreatic juice in bile duct through anomalous biliopancreatic union and long common channel. Presence of choledochal cyst with pancreas divisum rules out reflux as the only theory for choledochal cyst formation as most of pancreatic secretion drains through minor papilla which has no communication with biliary system [
7,
8]. Pancreas divisum has been implicated with acute pancreatitis in 25-38% patients [
7]. The incidence of acute pancreatitis with CC is 10-55% in adults and 0-70% in children [9]. CC with PD can be managed with pre-operative minor papilla sphincterotomy with or without stenting or trans-duodenal papillectomy followed by CC excision [
2,
8,
10]. Type 3 CC (choledochocele) with PD have been managed with either endoscopic sphincteroplasty or sphincterotomy as therapeutic modality by some authors [
11]. Till date no such case of left sided gall bladder with choledochal cyst and pancreas divisum has been reported as per search done in medical libraries -Pubmed, Cochrane, Google Scholar, Embase and Medline using Boolean operator “AND, AND” “AND, OR”. This anomaly mandates quick improvisation to avoid risk of biliovascular injuries compared to normally positioned gall bladder. In such case division of falciform ligament is necessary for unhampered fundal traction. Also direction of traction of infundibulum/neck of gall bladder will be down and left to open up and dissect hepatocystic triangle if cystic duct joins to left of CHD unlike in normal positioned gall bladder.
Conclusion
Identification of anomalies in HPB surgery pre-operatively by various set of investigations (MRCP, contrast enhanced MRI, CECT) can make us cautious and careful intra-operatively. Although LSG and CC with PD have been reported previously separately but this is first case report showing their association.
Contributors: VKS, RB: conception and design; VKS, DS: data collection; VKS, YVS, AC: analysis and interpretation; RB, VKS: drafting the article. AC will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study.
Funding: None; Competing interests: None stated.
References
- Abongwa HK, De Simone B, Alberici L, Iaria M, Perrone G, Tarasconi A, Baiocchi G, et al. Implications of left-sided gallbladder in the emergency setting: retrospective review and top tips for safe laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2017;27:220-227.
- Ransom-Rodríguez A, Blachman-Braun R, Sánchez-García Ramos E, Varela-Prieto J, Rosas-Lezama E, Mercado MÁ. A rare case of choledochal cyst with pancreas divisum: Case presentation and literature review. Ann Hepatobiliary Pancreat Surg. 2017;21:52-56.
- Pakkala A, Nagari B, Nekarakanti PK, Bansal AK. A case series of choledochal cyst with pancreatic divisum: A rare association. Turk J Surg. 2022;38:294-297.
- Maetani Y, Itoh K, Kojima N, Tabuchi T, Shibata T, Asonuma K, et al. Portal vein anomaly associated with deviation of the ligamentum teres to the right and malposition of the gallbladder. Radiology. 1998;207:723-728.
- Idu M, Jakimowicz J, Iuppa A, Cuschieri A. Hepatobiliary anatomy in patients with transposition of the gallbladder: implications for safe laparoscopic cholecystectomy. Br J Surg. 1996;83:1442-1443.
- Nagai M, Kubota K, Kawasaki S, Takayama T, Bandai Y, Makuuchi M. Are left-sided gallbladders really located on the left side? Ann Surg. 1997;225:274-280.
- Kuzel AR, Lodhi MU, Rahim M. Pancreatic divisum: An unusual cause of chronic pancreatitis in a young patient. Cureus. 2017;9:e1856.
- Arulprakash S, Balamurali R, Pugazhendhi T, Kumar SJ. Pancreas divisum and choledochal cyst. Indian J Med Sci. 2009;63:198-220.
- Fujishiro J, Masumoto K, Urita Y, Shinkai T, Gotoh C. Pancreatic complications in pediatric choledochal cysts. J Pediatr Surg. 2013;48:1897-1902.
- Tuggle DW, Smith EI. Pancreas divisum, pancreatic pseudocyst, and choledochal cyst in an 8-year-old child. J Pediatr Surg. 1989;24:52-53.
- Sonoda M, Sato M, Miyauchi Y, Yazumi S, Nakamura M. A rare case of choledochocele associated with pancreas divisum. Pediatr Surg Int. 2009;25:991-994.