|
SR Swarna1, Karaunakaran Vignesh2, S Vijayashankar3, Bharathi3, Jeyakumari1 Departments of 1Microbiology and 2Otorhinolaryngology, Karaikal, JIPMER, Puducherry, and 3Government General Hospital, Karaikal, Puducherry, India.
Corresponding Author:
Dr SR Swarna Email: srswa@yahoo.co.in
Abstract
Background: Mucormycosis is a fulminant fungal infection caused by members of the class Zygomycetes. These saprophytic fungi infect the immunocompromised hosts through inhalation of spores from soil. The most common presentation includes maxillary form of rhinocerebral mucormycosis with Rhizopus species isolated frequently. Case Report: Here, we document a case of a 57-year-old male with the complaints of maxillary swelling and pain. He had a history of diabetes with no medications taken for past few months. Based on the findings from the laboratory diagnosis, mucormycosis involving maxillary sinus was made. Conclusion: In the present case, high level of suspicion based on lab findings helped in proper management. Moreover, sooner recovery was possible due to the localized maxillary form of infection and good general health condition.
|
Introduction
Mucormycosis is a rapidly progressive lethal form of fungal infection seen in patients with uncontrolled diabetes and immunocompromised conditions. The prevalence of angio-invasive fungal infection in India is estimated to be at 0.02 to 9.5 cases (with a median of 0.2 cases) per 100,000 persons, nearly 70 times greater than the global data based on the computational model-based method [ 1]. A prevalence of 0.2-1.7% was reported in diabetic patients with mucormycosis [ 2]. The most frequently reported fungi were Rhizopus species, Apophysomyces spp, Lichtheimia spp and, less common fungi include Rhizomucor pusillus, Cunninghamella spp, Mucor spp, Syncephalastrum spp, and Saksenaea spp [ 3]. Mucormycosis is presented clinically as rhino-cerebral, pulmonary, gastrointestinal, cutaneous, central nervous system, or disseminated form [ 4]. The maxillary form of rhino-cerebral mucormycosis is the most common presentation of the head and neck region in a person with poorly controlled diabetes. Here, documenting a case of mucormycosis presented as maxillary form in a 57-year-old diabetic male patient from this region.
Case Report
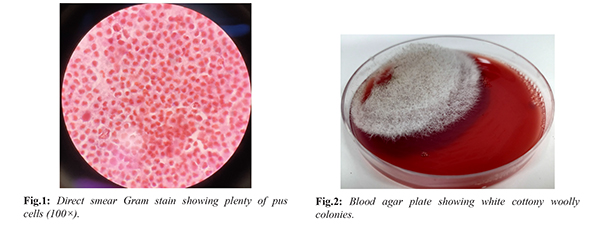
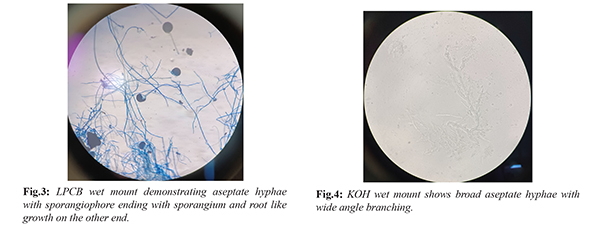
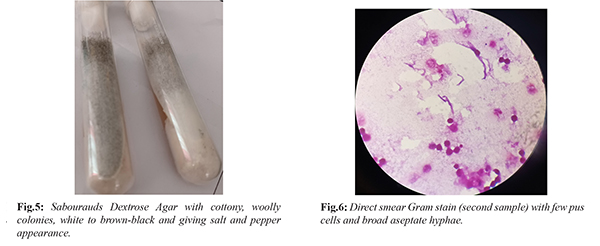
A 57-year-old male presented to the Otorhinolaryngology outpatient department of the Government General Hospital in this region with complaints of left-sided maxillary swelling and pain for the past week. He reported a history of intermittent fever with moderate pain but denied any headache, nasal congestion, purulent discharge, foul odor, or recent tooth extraction. The patient was a known case of type II diabetes mellitus, on oral hypoglycemic treatment for three years. However, he had discontinued his medications and avoided laboratory investigations for the past few months. On general examination, his vital signs were normal. He was provisionally diagnosed with facial cellulitis and initiated on antibiotics and supportive treatment. Biochemical investigations revealed elevated blood glucose levels, with fasting blood sugar at 315 mg/dL and post-prandial blood sugar at 390 mg/dL. By the third day of treatment, the patient's pain had reduced, and his blood sugar levels were controlled. A sublabial incision was performed, yielding approximately 6 mL of pus from the left maxillary sinus and buccal space abscess. The pus was sent for microbiological analysis. The macroscopic appearance of the pus was thick and purulent and showed plenty of pus cells with no bacteria on direct smear Gram stain [Fig.1]. Pus was also inoculated on Blood Agar (BA) and MacConkey agar (MAC) and incubated at 37°C. After 24 hours, no growth was noted, whereas 48 hours of incubation showed white cottony woolly colonies on BA [Fig.2] and no growth on MacConkey agar. LPCB wet mount of the colonies demonstrated broad aseptate hyaline hyphae with sporangiophore ending at sporangium and root-like growth at the nodes [Fig.3]. The KOH wet mount of the first sample also demonstrated broad aseptate hyphae with wide-angle branching [Fig.4]. As the growth resembles that of Rhizopus spp, leftover unprocessed sample was inoculated on Sabouraud Dextrose Agar (SDA) medium. On Day 5, SDA of the first sample showed cottony woolly colonies with tube filling growth, white to brown-black, and giving salt and pepper appearance [Fig.5]. LPCB wet mount of colonies from SDA revealed aseptate hyphae with sporangiophore containing sporangium and the presence of nodal rhizoids which confirms the etiology to be Rhizopus spp. To confirm the etiology, a second sample of aspirate (0.5 ml) was received on day-8 on request. Macroscopically, dried tissue material with little pus was noted and inoculated on SDA. The direct smear Gram stain showed few pus cells along with broad aseptate hyphae [Fig.6]. The KOH wet mount demonstrated broad aseptate hyphae with wide-angle branching. The laboratory findings along with clinical presentation are suggestive of Mucormycosis involving the maxillary sinus. The patient was referred to JIPMER, Puducherry, and started anti-fungal therapy. After two weeks of treatment with amphotericin B, the patient recovered well.
Discussion
Mucormycosis is a fulminant fungal infection and affects more commonly the immunocompromised host. These fungi are present in soil, air, food, animal excreta, and in the environment as saprophytes [5]. In a healthy individual, fungal spore enters through the inhalation route daily and colonize mucosa of the oral and nasal cavity, paranasal sinuses, and pharyngeal mucosa. The fungal spore also gets precipitated through trauma, dental extractions, intramuscular injections to infected wounds, insect bites, intravenous drug abuse, and prosthetic devices [ 5, 6]. In immunocompetent hosts, the intact cutaneous and mucosal epithelium and endothelium act as an effective barrier against tissue invasion and angioinvasion. Therefore, spores are contained by innate immune responses. When the fungal spores escape this mechanism, it is also likely to secrete several toxins or proteases and develop into hyphae after germination. These hyphae are resistant to killing by polymorphonuclear leukocytes. The impairment of the immune defense renders the host vulnerable to fungal colonization. Moreover, fungal hyphae show affinity towards arteries, veins, and lymphatics. It spreads to orbital and intracranial structures by either direct invasion or through blood vessels causing endothelial damage, thrombosis, and infarction. Further, this progresses towards ischemia and necrosis of deep tissues resulting in life-threatening fatal disease [ 7]. The present study documents a case of mucormycosis involving the maxillary sinus from this region. In India, there is a rise in the incidence of mucormycosis reported from 25 cases per year (1990-2007) to 89 cases per year (2013-2015) [8]. The reason put forth for the rising incidence was due to improved awareness and expertise in diagnosing the disease apart from the real rise in the incidence. A multicenteric study from India reported an annual incidence of 22 cases per year with an average of 38.8 cases for each center [9]. Few other studies from South India showed an annual incidence of 18.4 cases per year during 2005-2015 and 9.5 cases per year during 2015-2019 [4,10]. In India, other predisposing factors like climate, socio-economic, hygiene, poverty, malnourished and diagnostic delay also contribute to invasive fungal infection [11]. The occurrence of mucormycosis is associated with one or several of these risk factors such as diabetes mellitus with ketoacidosis, chronic renal insufficiency, hematological malignancy, organ transplant, malnutrition, increased serum iron, prolonged neutropenia or immunosuppressive drugs such as steroids, cytotoxic and broad-spectrum antibiotics, deferoxamine therapy [4,12]. However, in nearly 50% of mucormycosis patients, the most common risk factor was diabetes mellitus due to the increased availability of glucose, lower pH, acidotic environment in ketoacidosis, and impaired host defense mechanism [5,13]. In the present study, the patient was diabetic and presented with facial cellulitis involving the maxillary sinus. Clinically, mucormycosis is presented as rhino-orbital-cerebral (ROCM), pulmonary, gastrointestinal, cutaneous, renal, and disseminated mucormycosis based on anatomic location [4]. In India, ROCM type of head and neck region with maxillary and orbital cellulitis accounts for 77% of all cases of mucormycosis and is associated with inadequately controlled diabetes mellitus [9]. This rhinocerebral form is divided into two types based on their severity, highly fatal and invasive rhino-orbital-cerebral form and less fatal rhino-maxillary form [7]. It was also reported that the localized rhinomaxillary form is seen commonly if the colonized sporangiospores are larger than 10 µm [14,15]. In ROCM mucormycosis, Rhizopus arrhizus was most commonly isolated from India and globally. The reason suggested for Rhizopus arrhizus was due to the enzyme ketoreductase, produced by the fungus that uses the diabetic patient's ketone bodies [16]. However, there has been a reported rise in mucormycosis due to Rhizopus microsporus and Rhizopus homothallicus in recent reports [8,9]. In the present study, KOH wet mount of pus aspirate showed broad hyaline aseptate hyphae with irregular branching morphologically suggestive of member in Order Mucorales. Based on the SDA culture and LPCB wet mount, the fungus was identified as Rhizopus spp. Further, the LPCB wet mount revealed a shorter sporangiophore arising from stolon in the opposite direction of rhizoids with slight bending curvature and grayish brown. The Rhizoids are simply short with no branching, subequal in length, and grayish brown. Moreover, shallow Apophyses, conical to oblong ovoid columella with collarette, and brownish-black sporangia were morphologically suggestive of Rhizopus microsporus [17]. After the laboratory diagnosis of mucormycosis was made, the reversal of hyperglycemia, followed by debridement and antifungal therapy with amphotericin B was started. The present case is mucormycosis of the maxillary sinus which does not spread beyond the sinus and the reversal of hyperglycemia resulted in a good prognosis. The patient was followed up for three months and recovered well.
Conclusion
Mucormycosis is a highly fatal disease in diabetic patients due to their impaired host defense mechanism. A high level of suspicion and awareness helped in prompt diagnosis and appropriate treatment. Moreover, as the infection was localized, maxillary sinus mucormycosis and the general health condition was good, resulting in faster recovery.
Contributors: SRS: manuscript writing, patient management; KV: manuscript editing, patient management; SV, Bh, Jk: critical inputs into the manuscript. SRS will act as a study guarantor. All authors approved the final version of this manuscript and are responsible for all aspects of this study. Funding: None; Competing interests: None stated.
References - Prakash H, Chakrabarti A. Global epidemiology of mucormycosis. J Fungi. 2019;5:26.
- Dayal D, Jain P, Kumar R, Bakshi J, Menon P, Das A, et al. Clinical spectrum and outcome of invasive filamentous fungal infections in children with Type 1 diabetes: North Indian experience. Clin. Pediatr. Endocrinol. 2015;24:51-57.
- Prakash H, Chakrabarti A. Epidemiology of mucormycosis in India. Microorganisms. 2021;9:523.
- Priya P, Ganesan V, Rajendran T, Geni VG. Mucormycosis in a tertiary care center in South India: A 4-year experience. Indian J Crit Care Med. 2020;24:168-171.
- Cornely OA, Alastruey-Izquierdo A, Arenz D, Chen SCA, Dannaoui E, Hochhegger B, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis. 2019;19(12): e405-e421.
- Gholinejad Ghadi N, Seifi Z, Shokohi T, Aghili S, Nikkhah M, Vahedi Larijani L, et al. Fulminant mucormycosis of maxillary sinuses after dental extraction inpatients with uncontrolled diabetic: two case reports, J Mycol Méd. 2018;28(2):399-402.
- Arya S, Sharanamma B, Patil N, Anitha B, Bhateja S, Basavaraj. Rhino-maxillary form of mucormycosis causing sinusitis: a rare case report with review of literature. Journal of Oral Medicine, Oral Surgery, Oral Pathology and Oral Radiology. 2015;1(1):39-44.
- Prakash H, Ghosh AK, Rudramurthy SM, Singh, P, Xess I, Savio J, et al. A prospective multicenter study on mucormycosis in India: Epidemiology, diagnosis, and treatment. Med Mycol. 2019;57:395-402.
- Patel A, Kaur H, Xess I, Michael JS, Savio J, Rudramurthy S, et al. A multi-centre observational study on the epidemiology, risk factors, management and outcomes of mucormycosis in India. Clin Microbiol Infect. 2020;26:944.e9-944.e15.
- Manesh A, Rupali P, Sullivan MO, Mohanraj P, Rupa V, George B, et al. Mucormycosis-A clinico-epidemiological review of cases over 10 years. Mycoses. 2019;62:391-398.
- Michele DM, Fortuna G, Leuci S, Adamo D, Ruoppo E, Siano M, et al. Mucormycosis in immunocompetent patients: a case-series of patients with maxillary sinus involvement and a critical review of the literature. International Journal of Infectious Diseases. 2011;15:e533-e540.
- Singh AK, Singh R, Joshi SR, Misra A. Mucormycosis in COVID-19: A systematic review of cases reported worldwide and in India. Diabetes Metab Syndr. 2021;15:102-106.
- Prabhu S, Alqahtani M, Shehabi MA. A fatal case of rhinocerebral mucormycosis of the jaw after dental extractions and review of literature. J Infect Publ Health. 2017;11(3):301-303.
- Prabhu RM, Patel R. Mucormycosis and entomophthoramycosis: a review of the clinical manifestations, diagnosis and treatment. Clin Microbiol Infect. 2004;10(Suppl 1):31-47.
- Kontoyiannis DP, Lewis RE. Invasive zygomycosis: update on pathogenesis, clinical manifestations, and management. Infect Dis Clin North Am. 2006;20:581-607.
- Pandey A, Bansal V, Asthana AK, Trivedi V, Madan M, Das A. Maxillary osteomyelitis by mucormycosis: report of four cases. International Journal of Infectious Diseases. 2011;15:e66-e69.
- Zheng R, Chen G, Huang H, Liu X. A monograph of Rhizopus. Sydowia International Journal of Mycology. 2007;59(2):179-377.
|